Table of Contents
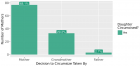
Awareness and Knowledge of Specialists/Trainers and General Dental Practitioners about Medical-Related Osteonecrosis of the Jaws
Published on: 13th November, 2024
Introduction: Bisphosphonate-related osteonecrosis of the jaw (BRONJ) was first reported in 2003. In 2014, it was revealed that not only bisphosphonates but also other antiresorptive and antiangiogenic drugs can cause osteonecrosis (Medication-related osteonecrosis of the jaw: MRONJ). The aim of this study is to compare awareness and knowledge about BRONJ and MRONJ among specialists/trainers (ST), general dental practitioners (GDP); and dentists who graduated before and after the year 2014. Materials and methods: A survey regarding demographic information and knowledge about BRONJ and MRONJ was prepared and delivered to dentists via social media.Results: A total of 422 dentists participated in our study. It was observed that the awareness and knowledge about BRONJ and MRONJ were statistically higher in ST and in dentists who graduated in 2014 or later. In addition, when their specialties were compared to each other, it was seen that the awareness and knowledge of Oral and Maxillofacial Radiologists (OMR) and Oral and Maxillofacial Surgeons (OMS) were higher than others.Discussion: According to the results of this study, it was seen that the awareness and knowledge of the ST group were higher than GDP, maybe because they may encounter these cases more. In addition, dentists who graduated in 2014 or later had higher awareness, maybe because MRONJ was coined and entered the dentistry education curriculum in 2014. Awareness and knowledge of OMR and OMS were found higher may be because they encounter these patients more frequently. Planning educational strategies for all dentists, especially GDP and dentists who graduated before 2014 is very important for post-graduate dentistry education.
Texture Analysis of Hard Tissue Changes after Sinus Lift Surgery with Allograft and Xenograft
Published on: 29th April, 2024
In the realm of dental surgery, implants are essential for replacing missing teeth. To facilitate implant placement, techniques such as bone grafting and sinus lifts are utilized to augment the volume of atrophied alveolar bone in candidates for dental implants. Typically, patients undergo a period of recovery following bone grafts before proceeding with implant placement. This study investigates the efficacy of Cone Beam Computed Tomography (CBCT) in measuring the residual bone volume and assessing bone quality after the healing phase. A texture analysis was conducted on CBCT scans from 42 patients requiring maxillary sinus lift reconstruction. These patients were categorized into two groups based on the type of grafting material used: Xenograft or allograft. The study analyzed the distribution of various texture parameters and conducted a Mann-Whitney U test to identify significant statistical differences between the groups. Results indicated non-normal distributions for specific variables such as Area_S(1,0) and S(1,0)SumOfSqs, while others like S(1,0)Entropy displayed normal distributions. The findings revealed no significant statistical differences in the primary outcomes between the xenograft and allograft groups. However, the average values of the gray shades of pixels in the allograft group were statistically significantly higher compared to the xenograft group, suggesting differences in bone texture post-procedure.
Advancing Oral Health and Craniofacial Science through Microchip Implants
Published on: 25th April, 2024
Microchip implants have emerged as transformative tools in the realm of oral health and craniofacial science, offering novel solutions to longstanding challenges. This paper aims to explore the diverse applications of microchip technology in dentistry and craniofacial medicine, envisioning a future where these implants play a pivotal role in diagnostics, treatment modalities, and ongoing patient care. The integration of microchips enables real-time monitoring of oral conditions, facilitating early detection of dental issues and providing personalized treatment strategies. Additionally, these implants open avenues for smart prosthetics and orthodontic devices, optimizing patient comfort and treatment outcomes. However, ethical considerations, patient perceptions, and the societal impact of such technology should also be addressed. By examining the multifaceted implications and applications of microchip implants in oral health and craniofacial science, this research overview seeks to contribute valuable insights to the intersection of technology and healthcare in the dental domain.
Hygiene and Care Protocols for Implant-supported Dental Prostheses in Patients with Diabetes
Published on: 21st February, 2024
Background: Prophylactic dental procedures following implant placement are critical to the long-term success of implants and are also dependent on the patient maintaining effective home care.Purpose: Evaluation of the effectiveness of preventive measures in patients with diabetes during long periods after prosthetic treatment with implants.Materials and methods: The study included 62 patients with diabetes with edentulism using 146 dental implants. Patients underwent constant monitoring, including regular occupational hygiene during follow-up examinations. Their frequency was set individually from 2 to 4 times A clinical index including Bleeding on Probing (BOP), Probing Depth (PD), and Marginal Bone Loss (MBL). Results: In patients included in the preventive protocol after 12 months, the mean BOP was 1.4 ± 0.15, and PPD was 2.46 ± 0.42. After 12 months in patients mean MBL was 0.72 ± 0.6 mm, after 3 years MBL was 1.24 ± 0.25 mm. For patients who were excluded from preventive services after 12 months, the mean BOP 1.9 ± 0.25, and the mean PPD was 3.56 ± 0.28). After 12 months in patients mean MBL was 0.87 ± 0.7 mm, after 3 years MBL was 1.52 ± 0.32 mm (p > 05). Compared to persons enrolled in the preventive protocol, those in the group without services were more likely to develop peri-implantitis (42.4% vs. 12,6%). The survival rate of implants after 3 years was 98.4%. The survival rate of implants in those patients who were excluded from preventive services after 3 years was 95.4%.Conclusion: For patients with diabetes, regular medical examinations, accompanied by professional oral hygiene procedures, prevent the development of negative reactions of the soft tissues surrounding the implant.
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial
Published on: 18th January, 2024
Background: Temporomandibular Disorder (TMD) pain attributed to myalgia is a common condition and patients should get advice on the best treatment option. Objectives: The aim was to evaluate the effect of two different exercise programs, or bite splint therapy, respectively, in patients with chronic frequent primary myofascial orofacial pain. Methods: The study was a randomized clinical trial including patients fulfilling criteria of chronic frequent primary myofascial orofacial pain with a reported pain intensity of ≥ 4 on a numerical rating scale (0-10). Ninety subjects were randomized to either bite splint, home exercises, or a supervised exercise program. Two examiners blinded to the treatment modality examined the same subject at baseline and a 3-month follow-up. Non-parametric statistical methods were applied for the outcome of treatment in intended-to-treat analyses. A P-value <0.05 was considered statistically significant. Results: The pain severity index was significantly reduced (p < 0.001) in all treatment groups. Jaw opening capacity improved significantly (p < 0.05) for those randomized to bite splint and for those in the home exercise program. About 70% of the participants reported improvement in their TMD pain severity with no significant difference between treatments. Both exercise groups improved in jaw function at the 3-month follow-up compared to baseline. Those who had a bite splint reported significantly more improvement in their headaches compared to those in the exercise programs. Conclusion: Jaw exercise programs and bite splint treatments had similar positive effects on TMD pain severity attributed to myalgia after 3 months.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."