More Information
Submitted: November 07, 2024 | Approved: November 12, 2024 | Published: November 13, 2024
How to cite this article: Koca AT, Bayhan M, Demir YA, Zengin AZ. Awareness and Knowledge of Specialists/Trainers and General Dental Practitioners about Medical-Related Osteonecrosis of the Jaws. J Oral Health Craniofac Sci. 2024; 9(1): 023-031. Available from: https://dx.doi.org/10.29328/journal.johcs.1001050.
DOI: 10.29328/journal.johcs.1001050
Copyright License: © 2024 Koca AT, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ); Medication-Related Osteonecrosis of the Jaw (MRONJ); Osteonecrosis; Awareness
Awareness and Knowledge of Specialists/Trainers and General Dental Practitioners about Medical-Related Osteonecrosis of the Jaws
Abdulhamit Taha Koca1, Mustafa Bayhan1, Yunus Ayberk Demir1 and Ayse Zeynep Zengin2*
1Ondokuzmayis University, Faculty of Dentistry, Samsun, Turkiye
2Ondokuzmayis University, Faculty of Dentistry, Oral and Maxillofacial Radiology, Samsun, Turkiye
*Address for Correspondence: Ayse Zeynep Zengin, Faculty of Dentistry, Ondokuzmayis University, Samsun, Turkiye, Email: [email protected]; [email protected]
Introduction: Bisphosphonate-related osteonecrosis of the jaw (BRONJ) was first reported in 2003. In 2014, it was revealed that not only bisphosphonates but also other antiresorptive and antiangiogenic drugs can cause osteonecrosis (Medication-related osteonecrosis of the jaw: MRONJ).
The aim of this study is to compare awareness and knowledge about BRONJ and MRONJ among specialists/trainers (ST), general dental practitioners (GDP); and dentists who graduated before and after the year 2014.
Materials and methods: A survey regarding demographic information and knowledge about BRONJ and MRONJ was prepared and delivered to dentists via social media.
Results: A total of 422 dentists participated in our study. It was observed that the awareness and knowledge about BRONJ and MRONJ were statistically higher in ST and in dentists who graduated in 2014 or later. In addition, when their specialties were compared to each other, it was seen that the awareness and knowledge of Oral and Maxillofacial Radiologists (OMR) and Oral and Maxillofacial Surgeons (OMS) were higher than others.
Discussion: According to the results of this study, it was seen that the awareness and knowledge of the ST group were higher than GDP, maybe because they may encounter these cases more. In addition, dentists who graduated in 2014 or later had higher awareness, maybe because MRONJ was coined and entered the dentistry education curriculum in 2014. Awareness and knowledge of OMR and OMS were found higher may be because they encounter these patients more frequently.
Planning educational strategies for all dentists, especially GDP and dentists who graduated before 2014 is very important for post-graduate dentistry education.
Bisphosphonates are antiresorptive drugs used in the treatment of metabolic and metastatic bone diseases, Paget’s, multiple myeloma, etc. One of the most important side effects associated with the use of bisphosphonates is osteonecrosis. The case of bisphosphonate-related osteonecrosis of the jaw (BRONJ) was first reported in 2003 by Marx [1]. In 2004, manufacturers of pamidronic acid and zolendronic acid, notified healthcare professionals that the risk of BRONJ was listed on their labels [2]. In 2005, this was extended to all bisphosphonates, including oral preparations. Warnings also appeared in the British National Formulary from 2008 [3]. The American Association of Oral and Maxillofacial Surgeons (AAOMS), in their article published in 2009, defined ‘bisphosphonate manufacturing osteonecrosis of the jaw’ as an exposed bone image lasting more than 8 weeks. It was observed in the jaws of patients who have not previously received radiotherapy in the head and neck area, and who have used or are using bisphosphonates [4].
In 2014, medications (monoclonal antibodies and tyrosine kinase inhibitors, in particular, denosumab, bevacizumab, and sunitinib) other than bisphosphonates have been found to cause MRONJ both spontaneously and following extraction. Patients, who do not have a history of radiotherapy or metastatic disease in the jaws, have been or are being treated with antiresorptive or antiangiogenic drugs, and have an intraoral or extraoral probable fistula lasting more than 8 weeks or exposed bone can be considered as MRONJ [5].
The AAOMS emphasizes the importance of consulting the patients with dentists and maintaining oral hygiene before the antiresorptive or antiangiogenic therapy [5,6]. The increasing number of patients using these drugs increases the rate of dentists encountering MRONJ. Thus, it is important for dentists to know the diagnosis and risk factors in order to prevent this type of necrosis.
In the literature, there are several studies carried out in different geographical areas, including dental students, GDP, oral and maxillofacial surgeons, prescribers, and patients, in an attempt to identify the level of knowledge, awareness, and clinical experience about BRONJ and MRONJ [7-11]. There is only one study that investigated the awareness and knowledge of dentists who are currently studying in different specialty/doctoral programs [12]. However, to our knowledge, there is no study carrying out dentists’ graduation date in terms of being aware of MRONJ coined in 2014 and comparing different specialties in the same study.
Therefore, this study aimed to compare awareness and knowledge about BRONJ and MRONJ among Specialists/Trainers (ST), General Dental Practitioners (GDP); and dentists who graduated before and after the year 2014.
A survey form, prepared via Google Forms, consists of 12 questions for dentists. The form included demographic information, year of graduation from the faculty of dentistry, specialization status, diagnosis, and treatment of BRONJ and MRONJ was prepared based on the 2014 position paper of AAOMS [5] and previous studies on this subject [13-15] (Table 1).
According to the power analysis, the minimum number of participants required at 95% test power was determined as 415. Ethics committee approval was obtained. (OMUKAEK:2023/490)
The survey form was delivered to dentists residing in Turkiye through social media. The survey was terminated when it reached 422 participants. Data were analyzed with IBM SPSS V23. Pearson’s Chi-square test was applied to the survey results. The chi-square test and Yates correction were used to compare categorical variables according to groups. Analysis results were presented as frequency (percentage) for categorical data. The significance level was taken as p < 0.050.
A total of 422 dentists, 160 men, and 262 women, participated in our study. Number of women participants was significantly higher than that of men (p < 0.05).
When we examined the distribution of gender and dentists’ encountering a case diagnosed with BRONJ and/or MRONJ, a statistically significant difference was found. (p = 0,021) Male dentists encountered more cases diagnosed with BRONJ or MRONJ than female dentists. However, when examining the distribution of gender and dentists’ knowledge about drugs that may cause MRONJ (p = 0,009) and knowing the risk factors (p = 0,002), female dentists responded more accurately than male dentists. No more statistically significant difference was observed between genders with other data.
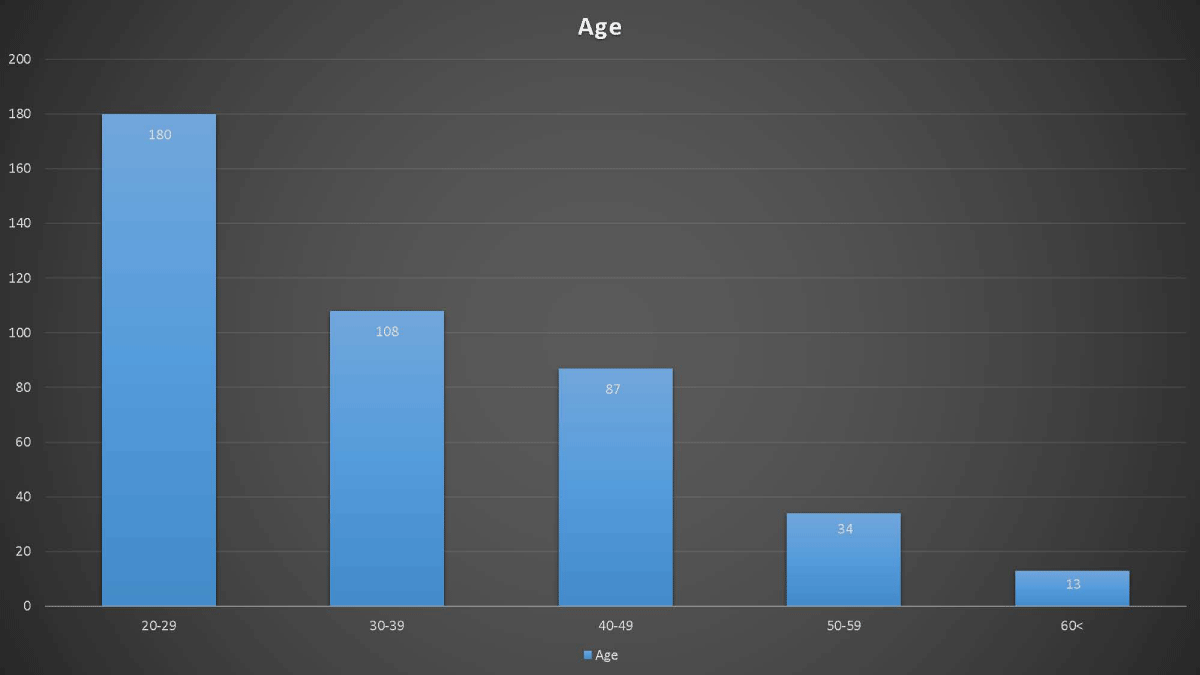
The age distribution of dentists participating in the survey is presented in Figure 1. 56.4% (n = 238) of the participants in the study graduated from the faculty of dentistry in 2014 or later, and 43.6% (n = 184) before 2014.
Figure 1: Age distribution of dentists participating in the survey.
While 92.4% of dentists have heard of BRONJ, 81.3% have heard of MRONJ. It was observed that only 57.1% of them knew the difference between BRONJ and MRONJ.
When the answers to the survey questions were examined, the following findings were obtained:
- A statistically significant differences were found between the graduation period and most of the survey questions (Table 1). According to these results, it was seen that dentists who graduated in 2014 or later had better awareness and knowledge about BRONJ and MRONJ than dentists who graduated before 2014. Of those who participated in the survey, 229 (54.1%) were specialists and Speciality Trainers (ST) and 193 (45.9%) were GDP.
- Have you ever heard of BRONJ?
- (1,7)
- Have you ever heard of MRONJ?
- Do you know the difference between BRONJ and MRONJ?
- Have you read any articles or scientific studies about BRONJ and/or MRONJ in the last five years?
- Have you experienced any patients with BRONJ and/or MRONJ?
- Have you ever received a consultation to ensure a patient's dental hygiene before using any medication that may cause BRONJ and/or MRONJ?
- In which part of the jaw does MRONJ occur more frequently?
| Table 1: Comparison of dentists' graduation year and specialization status and awareness about BRONJ and MRONJ. | ||||||
| QUESTIONS | ST | GDP | p -Value | Graduated before 2014 | Graduated in and after 2014 | p -Value |
| 0,004y | <0,001y | |||||
| Yes | 220 (96,1) | 170 (88,1) | 156 (84,8) | 234 (98,3) | ||
| No | 9 (3,9) | 23 (11,9) | 28 (15,2) | |||
| 0,003x | <0,001x | |||||
| Yes | 198 (86,5) | 145 (75,1) | 128 (69,6) | 215 (90,3) | ||
| No | 31 (13,5) | 48 (24,9) | 56 (30,4) | 23 (9,7) | ||
| <0,001x | <0,001x | |||||
| Yes | 156 (68,1) | 85 (44) | 72 (39,1) | 169 (71) | ||
| No | 73 (31,9) | 108 (56) | 112 (60,9) | 69 (29) | ||
| <0,001x | 0,159x | |||||
| Yes | 122 (53,3) | 71 (36,8) | 77 (41,9) | 116 (48,7) | ||
| No | 107 (46,7) | 122 (63,2) | 107 (58,2) | 122 (51,3) | ||
| <0,001x | 0,887x | |||||
| Yes | 150 (65,5) | 81 (42) | 100 (54,4) | 131 (55) | ||
| No | 79 (34,5) | 112 (58) | 84 (45,7) | 107 (45) | ||
| <0,001x | 0,822x | |||||
| Yes | 109 (47,6) | 38 (19,7) | 63 (34,2) | 84 (35,3) | ||
| No | 120 (52,4) | 155 (80,3) | 121 (65,8) | 154 (64,7) | ||
| <0,001x | <0,001x | |||||
| Maxilla | 9 (3,9) | 10 (5.2) | 11 (5.9) | 8 (3.4) | ||
| I don't know | 48 (21) | 83 (43) | 84 (45,7) | 47 (19,7) | ||
| Mandible | 172 (75,1) | 100 (51.8) | 89 (48.4) | 183(76.9) | ||
| 8. Which route of medication administration increases the risk of MRONJ?" | <0,001x | <0,001x | ||||
| I don't know | 42 (18,3) | 70 (36,3) | 71 (38,6) | 41 (17,2) | ||
| There is no difference | 9 (3,9) | 24 (12,4) | 19 (10,3) | 14 (5,9) | ||
| IM | 6 (2,6) | 7 (3,6) | 6 (3,3) | 7 (2,9) | ||
| IV | 164 (71,6) | 85 (44) | 78 (42,4) | 171 (71,9) | ||
| Oral | 8 (3,5) | 7 (3,6) | 10 (5,4) | 5 (2,1) | ||
| 9. Do you know the treatment procedure in cases of MRONJ? | <0,001x | <0,001x | ||||
| Yes | 107 (46,7) | 60 (31,1) | 53 (28,8) | 114 (47,9) | ||
| No | 122 (53,3) | 133 (68,9) | 131 (71,2) | 124 (52,1) | ||
| 10. Which are known risk factors related to MRONJ? | <0,001x | <0,001x | ||||
| Do not know | 24 (10,5) | 47 (24,4) | 47 (25,5) | 24 (10,1) | ||
| Gender | 64 (27,9) | 38 (19,7) | 36 (19,6) | 66 (27,7) | ||
| Diabetes mellitus | 111 (48,5) | 78 (40,4) | 77 (41,8) | 112 (47,1) | ||
| Hypertension | 27 (11,8) | 18 (9,3) | 14 (7,6) | 31 (13) | ||
| Hypothyroidism | 33 (14,4) | 15 (7,8) | 16 (8,7) | 32 (13,4) | ||
| Invasive dental procedures | 152 (66,4) | 72 (37,3) | 77 (41,8) | 147 (61,8) | ||
| Prior cancer history | 158 (69) | 105 (54,4) | 93 (50,5) | 170 (71,4) | ||
| Comedication with corticosteroids | 131 (57,2) | 80 (41,5) | 82 (44,6) | 129 (54,2) | ||
| Age | 113 (49,3) | 68 (35,2) | 73 (39,7) | 108 (45,4) | ||
| 11. Which medications can cause MRONJ? | <0,001x | <0,001x | ||||
| Analgesics | 1 (0,4) | 1 (0,5) | 1 (0,5) | 1 (0,4) | ||
| Antiplatelet drugs | 1 (0,4) | 2 (1) | 1 (0,5) | 2 (0,8) | ||
| Angiogenesis inhibitors | 85 (37,1) | 30 (15,5) | 40 (21,7) | 75 (31,5) | ||
| Antibiotics | 0 (0) | 3 (1,6) | 2 (1,1) | 1 (0,4) | ||
| Antihypertensive drugs | 4 (1,7) | 2 (1) | 0 (0) | 6 (2,5) | ||
| Antiresorptive drugs | 129 (56,3) | 77 (39,9) | 72 (39,1) | 134 (56,3) | ||
| Bisphosphonates | 214 (93,4) | 166 (86) | 151 (82,1) | 229 (96,2) | ||
| Do not know | 11 (4,8) | 18 (9,3) | 24 (13) | 5 (2,1) | ||
| Oral contraceptive pills | 16 (7) | 19 (9,8) | 7 (3,8) | 28 (11,8) | ||
| 12. Which dental procedures can cause MRONJ? | <0,005x | <0,001x | ||||
| Tooth extraction | 216 (94,3) | 160 (82,9) | 150 (81,5) | 226 (95) | ||
| Removable partial dentures | 36 (15,7) | 35 (18,1) | 36 (19,6) | 35 (14,7) | ||
| Dental implants | 190 (83) | 159 (82,4) | 143 (77,7) | 206 (86,6) | ||
| Root-canal treatment | 42 (18,3) | 34 (17,6) | 37 (20,1) | 39 (16,4) | ||
| Orthodontic treatment | 28 (12,2) | 39 (20,2) | 23 (12,5) | 44 (18,5) | ||
| Dental crowns | 5 (2,2) | 4 (2,1) | 2 (1,1) | 7 (2,9) | ||
| Supragingival scaling | 37 (16,2) | 37 (19,2) | 33 (17,9) | 41 (17,5) | ||
| BRONJ: Bisphosphonate-Related Osteonecrosis of the Jaw; MRONJ: Medication-Related Osteonecrosis of the Jaw; ST: Specialists/Trainers; GDP: General Dental Practitioners; IV: Intravenous; IM: Intramuscular | ||||||
- A statistically significant differences were found between ST and GDP in all of the survey questions (Table 1). According to these results, it was seen that awareness and knowledge levels of ST about BRONJ and MRONJ are higher than GDP.
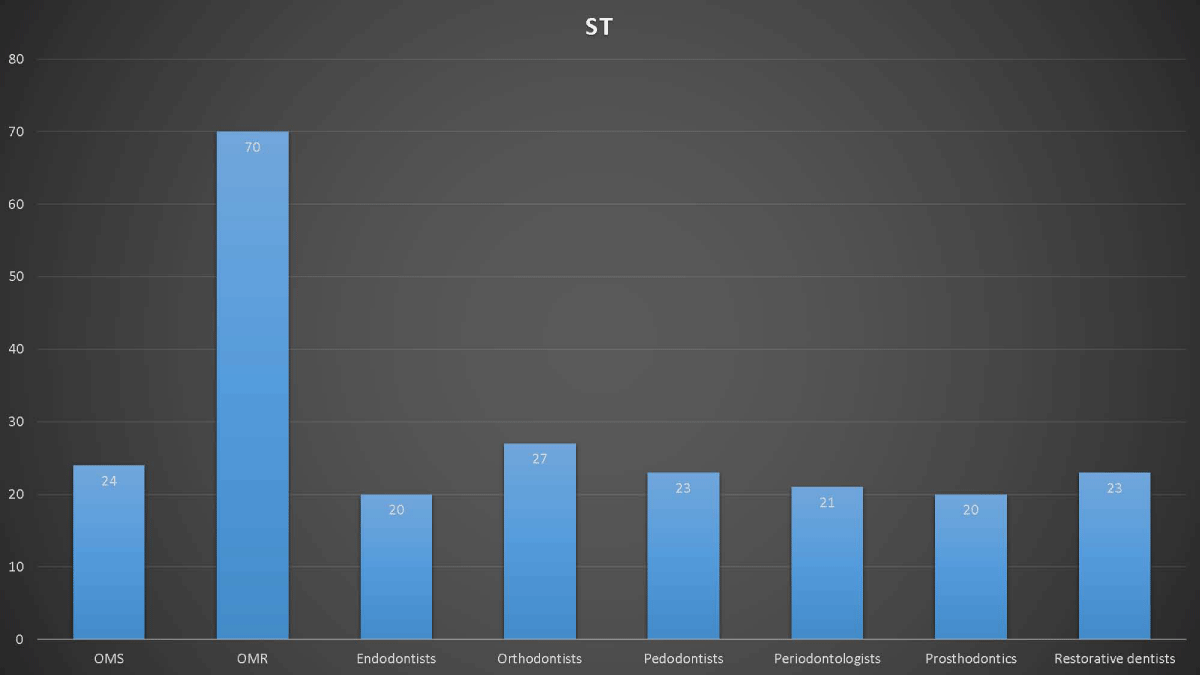
- The distribution and percentage of ST group by areas of expertise are shown in Figure 2. 96.5% of ST have heard of BRONJ and there was no statistically significant difference in terms of having heard of BRONJ beforehand and also regarding their areas of expertise (p = 0.060). However, when we compare all other data according to areas of expertise, statistically significant differences were found among them (p < 0.001)/(p = 0.001) (Table 2).
- In addition, when we compare the data on knowing the treatment procedure in MRONJ cases according to the fields of expertise, a difference was found between Oral and Maxillofacial Surgeons (OMS) and Endodontists, Orthodontists, Pedodontists, Periodontists, Prostodontists and Restorative Dentists. Also, a difference was observed between Oral and Maxillofacial Radiologists (OMR) and Orthodontists, Pedodontists, Prostodontists and Restorative dentists.
- Accordingly, it was seen that OMR and OMS have higher knowledge and awareness of MRONJ than other specialties.
Figure 2: The distribution and percentage of specialities and speciality trainers according to the areas of expertise.
| Table 2: Comparison of dentists' awareness of MRONJ according to their specialties. | ||||||||||
| Questions | OMS | OMR | Endodontists | Orthodontists | Pedodontists | Periodontologists | Prosthodontists | Restorative Dentists | Total | p |
| 1. Have you heard of BRONJ?* | 0,060 x | |||||||||
| Yes | 23 (95,8) | 69 (98,6) | 20 (100) | 23 (85,2) | 22 (95,7) | 20 (95,2) | 20 (100) | 23 (100) | 220 (96,5) | |
| No | 1 (4,2) | 1 (1,4) | 0 (0) | 4 (14,8) | 1 (4,4) | 1 (4,8) | 0 (0) | 0 (0) | 8 (3,5) | |
| 2. Have you heard of MRONJ?* | <0,001x | |||||||||
| Yes | 24 (100) | 69 (98,6) | 18 (90) | 20 (74,1) | 16 (69,6) | 16 (76,2) | 14 (70) | 21 (91,3) | 198 (86,8) | |
| No | 0 (0) | 1 (1,4) | 2 (10) | 7 (25,9) | 7 (30,4) | 5 (23,8) | 6 (30) | 2 (8,7) | 30 (13,2) | |
| 3. Do you know the difference between BRONJ and MRONJ?* | <0,001 x | |||||||||
| Yes | 22 (91,7) | 65 (92,9) | 12 (60) | 14 (51,8) | 8 (34,8) | 13 (61,9) | 8 (40) | 14 (60,9) | 156 (68,4) | |
| No | 2 (8,3) | 5 (7,1) | 8 (40) | 13 (48,2) | 15 (65,2) | 8 (38,1) | 12 (60) | 9 (39,1) | 72 (31,6) | |
| 4. Have you read any articles or scientific studies about BRONJ and/or MRONJ in the last five years?* | <0,001 x | |||||||||
| Yes | 21 (87,5) | 59 (84,3) | 10 (50) | 4 (14,8) | 5 (21,7) | 12 (57,1) | 4 (20) | 7 (30,4) | 122 (53,5) | |
| No | 3 (12,5) | 11 (15,7) | 10 (50) | 23 (85,2) | 18 (78,3) | 9 (42,9) | 16 (80) | 16 (69,6) | 106 (46,5) | |
| 5. Have you experienced any patients with BRONJ and/or MRONJ?* | <0,001 x | |||||||||
| Yes | 23 (95,8) | 65 (92,9) | 10 (50) | 8 (29,6) | 9 (39,1) | 13 (61,9) | 12 (60) | 10 (43,5) | 150 (65,8) | |
| No | 1 (4,2) | 5 (7,1) | 10 (50) | 19 (70,4) | 14 (60,9) | 8 (38,1) | 8 (40) | 13 (56,5) | 78 (34,2) | |
| 6. Have you ever received a consultation to ensure a patient's dental hygiene before using any medication that may cause BRONJ and/or MRONJ?* | <0,001 x | |||||||||
| Yes | 19 (79,2) | 49 (70) | 12 (60) | 1 (3,7) | 4 (17,4) | 8 (38,1) | 5 (25) | 11 (47,8) | 109 (47,8) | |
| No | 5 (20,8) | 21 (30) | 8 (40) | 26 (96,3) | 19 (82,6) | 13 (61,9) | 15 (75) | 12 (52,2) | 119 (52,2) | |
| 7. In which area of the jaw does MRONJ occur more frequently?* | <0,001x | |||||||||
| I don't know | 0 (0) | 4 (5,7) | 5 (25) | 9 (33,3) | 9 (39,1) | 3 (14,3) | 9 (45) | 8 (34,8) | 47 (20,6) | |
| Maxilla | 1 (4,2) | 2 (2,9) | 1 (5) | 0 (0) | 2 (8,7) | 0 (0) | 1 (5) | 2 (8,7) | 9 (4) | |
| Mandible | 23 (95.8) | 64 (91.4) | 14 (70) | 18 (66.7) | 12 (52,2) | 18 (85.7) | 10 (50) | 13 (56.5) | 172(75.4) | |
| 8. Which route of medication administration increases the risk of MRONJ?" | 0,001^ | |||||||||
| I don't know | 1 (4,2) | 2 (2,9) | 4 (20) | 8 (29,6) | 9 (39,1) | 3 (14,3) | 5 (25) | 10 (43,5) | 42 (18,4) | |
| There is no difference | 0 (0) | 2 (2,9) | 1 (5) | 1 (3,7) | 1 (4,4) | 0 (0) | 1 (5) | 2 (8,7) | 8 (3,5) | |
| IM | 0 (0) | 2 (2,9) | 0 (0) | 0 (0) | 1 (4,4) | 0 (0) | 1 (5) | 2 (8,7) | 6 (2,6) | |
| IV | 23 (95,8) | 63 (90) | 15 (75) | 16 (59,3) | 11 (47,8) | 17 (81) | 12 (60) | 7 (30,4) | 164 (71,9) | |
| Oral | 0 (0) | 1 (1,4) | 0 (0) | 2 (7,4) | 1 (4,4) | 1 (4,8) | 1 (5) | 2 (8,7) | 8 (3,5) | |
| 9. Do you know the treatment procedure in cases of MRONJ?* | <0,001 x | |||||||||
| Yes | 23 (95,8) | 50 (71,4) | 8 (40) | 2 (7,4) | 3 (13) | 11 (52,4) | 4 (20) | 6 (26,1) | 107 (46,9) | |
| No | 1 (4,2) | 20 (28,6) | 12 (60) | 25 (92,6) | 20 (87) | 10 (47,6) | 16 (80) | 17 (73,9) | 121 (53,1) | |
| 10. Which are known risk factors related to MRONJ?* | 0,001 x | |||||||||
| Do not know | 0 (0) | 2 (2,9) | 3 (15) | 6 (22,2) | 6 (26,1) | 0 (0) | 4 (20) | 3 (13) | 24 (10,5) | |
| Gender | 8 (33,3) | 22 (31,4) | 8 (40) | 6 (22,2) | 6 (26,1) | 5 (23,8) | 4 (20) | 4 (17,4) | 63 (27,6) | |
| Diabetes mellitus | 12 (50) | 42 (60) | 10 (50) | 11 (40,7) | 10 (43,5) | 8 (38,1) | 5 (25) | 12 (52,2) | 110 (48,2) | |
| Hypertension | 2 (8,3) | 10 (14,3) | 2 (10) | 3 (11,1) | 2 (8,7) | 1 (4,8) | 1 (5) | 6 (26,1) | 27 (11,8) | |
| Hypothyroidism | 3 (12,5) | 12 (17,1) | 4 (20) | 4 (14,8) | 2 (8,7) | 2 (9,5) | 2 (10) | 4 (17,4) | 33 (14,5) | |
| Invasive dental procedures | 17 (70,8) | 53 (75,7) | 12 (60) | 14 (51,9) | 10 (43,5) | 16 (76,2) | 13 (65) | 17 (73,9) | 152 (66,7) | |
| Prior cancer history | 21 (87,5) | 51 (72,9) | 15 (75) | 15 (55,6) | 13 (56,5) | 14 (66,7) | 10 (50) | 18 (78,3) | 157 (68,9) | |
| Comedication with corticosteroids | 12 (50) | 47 (67,1) | 11 (55) | 9 (33,3) | 12 (52,2) | 13 (61,9) | 11 (55) | 15 (65,2) | 130 (57) | |
| Age | 12 (50) | 48 (68,6) | 9 (45) | 12 (44,4) | 10 (43,5) | 5 (23,8) | 7 (35) | 9 (39,1) | 112 (49,1) | |
| 11. Which medications can cause MRONJ? | <0,001 x | |||||||||
| Analgesics | 0 (0) | 1 (1,4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (0,4) | |
| Antiplatelet drugs | 0 (0) | 1 (1,4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (0,4) | |
| Angiogenesis inhibitors | 14 (58,3) | 42 (60) | 2 (10) | 4 (14,8) | 6 (26,1) | 4 (19) | 4 (20) | 9 (39,1) | 85 (37,3) | |
| Antibiotics | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Antihypertensive drugs | 0 (0) | 0 (0) | 0 (0) | 1 (3,7) | 0 (0) | 0 (0) | 0 (0) | 3 (13) | 4 (1,8) | |
| Antiresorptive drugs | 21 (87,5) | 57 (81,4) | 9 (45) | 7 (25,9) | 6 (26,1) | 12 (57,1) | 8 (40) | 8 (34,8) | 128 (56,1) | |
| Bisphosphonates | 23 (95,8) | 68 (97,1) | 20 (100) | 22 (81,5) | 21 (91,3) | 20 (95,2) | 18 (90) | 21 (91,3) | 213 (93,4) | |
| Do not know | 0 (0) | 0 (0) | 0 (0) | 5 (18,5) | 2 (8,7) | 1 (4,8) | 1 (5) | 2 (8,7) | 11 (4,8) | |
| Oral contraceptive pills | 1 (4,2) | 5 (7,1) | 2 (10) | 2 (7,4) | 0 (0) | 0 (0) | 2 (10) | 4 (17,4) | 16 (7) | |
| 12. Which dental procedures can cause MRONJ?* | 0,001 x | |||||||||
| Tooth extraction | 23 (95,8) | 67 (95,7) | 20 (100) | 23 (85,2) | 20 (87) | 21 (100) | 20 (100) | 21 (91,3) | 215 (94,3) | |
| Removable partial dentures | 6 (25) | 14 (20) | 3 (15) | 1 (3,7) | 3 (13) | 5 (23,8) | 0 (0) | 4 (17,4) | 36 (15,8) | |
| Dental implants | 22 (91,7) | 61 (87,1) | 18 (90) | 18 (66,7) | 18 (78,3) | 19 (90,5) | 17 (85) | 16 (69,6) | 189 (82,9) | |
| Root-canal treatment | 2 (8,3) | 10 (14,3) | 5 (25) | 12 (44,4) | 3 (13) | 3 (14,3) | 3 (15) | 4 (17,4) | 42 (18,4) | |
| Orthodontic treatment | 5 (20,8) | 6 (8,6) | 6 (30) | 0 (0) | 5 (21,7) | 3 (14,3) | 0 (0) | 3 (13) | 28 (12,3) | |
| Dental crowns | 1 (4,2) | 1 (1,4) | 2 (10) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4,3) | 5 (2,2) | |
| Supragingival scaling | 7 (29,2) | 7 (10) | 4 (20) | 6 (22,2) | 4 (17,4) | 4 (19) | 4 (20) | 1 (4,3) | 37 (16,2) | |
| xPearson’s Chi Squared Test ; n(%), *multiple response BRONJ: Bisphosphonate-Related Osteonecrosis of the Jaw; MRONJ: Medication-Related Osteonecrosis of the Jaw; ST: Specialists/Trainers; GDP: General Dental Practitioners; IV: Intravenous; IM: Intramuscular; OMS: Oral and Maxillofacial Surgions; OMR: Oral and Maxillofacial Radiologists |
||||||||||
The first case of BRONJ due to the use of bisphosphonates was reported in 2003. In 2014, AAOMS changed the term BRONJ to MRONJ stating that not only bisphosphonates but also other antiresorptive and antiangiogenic drugs play a role in the cases of necrosis [5]. That is why the aim of this study is to compare the awareness and knowledge of dentists who graduated before and in 2014 or later, about BRONJ and MRONJ. The study performed by Patil, et al. [13] amongst dentists to evaluate their knowledge and awareness regarding MRONJ and its management showed that most dentists lack adequate information. Ekici Ö [15] reported that more than half of the dentists in their study were unable to define osteonecrosis of the jaw. Most (61.2%) were able to identify bisphosphonates associated with MRONJ, but about 80% were unaware of antiangiogenic drugs. Tanna, et al. [11] mentioned that more than 90% of the GDP was unaware of anti-resorptive and anti-angiogenic medications other than bisphosphonates that had the potential to cause MRONJ. Landi, et al. [16] revealed that about half of the interviewed dentists admit an insufficient or barely sufficient knowledge of the matter. Al-Samman & Al-Ani [8], in 2019, reported that only 33% of GDP claim to have adequate knowledge about MRONJ. Aslan, et al. [12], in 2022, reported the highest rate, 95% of speciality trainers (PDSs) had knowledge about MRONJ. On the other hand, when the PDSs were asked about the definition of MRONJ suggested by the 2014 position paper of the AAOMS, only 52.5% answered this question correctly. In this study, dentists have heard of BRONJ (92.2%) more than MRONJ (81.1 %). Only 57% of dentists know the difference between BRONJ and MRONJ. More than half of GDP (56%) and dentists who graduated before 2014 (60.9%) could not know the difference between BRONJ and MRONJ.
Landi, et al. [16] reported that one or more MRONJ-affected patients were encountered by 63.2% of the respondents. Aslan, et al. [12] reported that only 38.5% of PDSs stated that a patient was referred to them for dental consultation before antiresorptive therapy; and 14% for antiangiogenic therapy. In this study, although 65.5% of ST and 42% of GDP had witnessed cases of MRONJ, only 47.6% of the ST and 19.7% of GDP received consultation from a medical doctor.
Awareness of the risks associated with MRONJ is important because that is a multifactorial disease for which aetiology is not fully understood. Demographic and systemic factors and different medications are variably reported as risk factors [17-19]. Patil, et al. [13] reported that 61.5% of dentists had no knowledge about risk factors associated with MRONJ. Ekici Ö [15] mentioned that most dentists in his study were unaware of most of the main risk factors for MRONJ.
Also, corticosteroids increase the risk for MRONJ when given in conjunction with antiresorptive agents [16]. Aslan, et al. [12] reported that corticosteroid therapy was identified only by 13.5%. Similarly, in a study, less than a third (29.7%) of the participants were aware that concomitant corticosteroid therapy may increase the risk of developing MRONJ [20]. In this study, more than half the rate of ST and dentists who graduated in 2014 or later marked corticosteroids among MRONJ risk factors.
MRONJ is more prevalent in patients receiving high cumulative doses and high-potency medications. About 90% of necrosis cases are seen in cancer patients receiving a high dose of IV therapy [21]. In this study, 71.6% of ST and 71.9% of dentists who graduated in 2014 or later, answered the question “Which of the drug use methods increases the risk of MRONJ formation?” correctly according to AAOMS 2014.
Limited information regarding anatomic risk factors for MRONJ is available. MRONJ is more likely to appear in the mandible (75%) than the maxilla (25%) but can appear in both jaws (4.5%) [17,22]. In this study while 75.1% of ST and 76,9% of dentists graduated in 2014 and later answered mandible, 43% of GDP and 45.7% of dentists who graduated before 2014 answered “I don’t know”.
Among cancer patients with MRONJ, preexisting inflammatory dental disease such as periodontal disease or periapical pathology was a risk factor among 50 percent of the cases [17,18]. Several studies have reported that in patients with MRONJ, tooth extraction is a common predisposing event, with 52 to 61% of patients reporting tooth extraction as the precipitating event [17,19]. Aslan, et al. [12] and el Aid, et al. [7] reported that the most cited risk factor regarding MRONJ was dentoalveolar surgery. In contrast to these investigations, the most cited risk factor regarding MRONJ was cancer history in this study. (69% of ST and 71% of dentists graduated in 2014 and after). 66.4% of ST and 61.8% of dentists who graduated in 2014 or later marked invasive dental procedures among MRONJ risk factors.
Strategies for treatment of patients at risk of or with MRONJ were presented in the AAOMS Position Papers in 2007, 2009, 2014 and 2022 [5,6]. Tanna, et al. [11] reported that there are many GDP who do not trust their knowledge regarding the treatment of patients taking bisphosphonates [23]. A study reported that 36% of dentists had received MRONJ training during their undergraduate education [15]. Acharya, et al. [14] reported that most of the participants (73%) responded that they had inadequate knowledge about its management guidelines. However, research from the British Dental Association in 2012 showed that 41% of GDP in the United Kingdom had qualified from either the European Economic Area or overseas [24]. In this study, 46.7% of the ST, 31.1% of the GDP, 28.8% of dentists who graduated before 2014, and 47.9% of those who graduated in 2014 or later know the treatment procedure. This finding supports Landi, et al. [16] that younger dentists are more aware of treatment procedures, however, in our opinion, post-graduate education is required for all ages of dentists.
Ekmekcioglu, et al. [25] conducted a questionnaire among GDP and specialists and showed that the latter were significantly more aware of MRONJ. Alhussain, et al. [26] reported that specialist dentists were more knowledgeable about MRONJ than general dentists. The other aim of this study was to compare the awareness and knowledge levels of the ST and GDP about BRONJ and MRONJ. ST group has heard of BRONJ and MRONJ at a rate of 96.1%, and 86.5%, respectively. According to the findings of this study, when we compare the knowledge level of ST and GDP about BRONJ and MRONJ, ST has higher awareness and knowledge. This result supports that postgraduate dental training is an effective factor for the dentists’ knowledge levels about MRONJ [25].
Many studies in the literature acknowledge that recently graduated younger dentists are more knowledgeable about MRONJ because MRONJ-related dental education is a recent concept in the undergraduate dentistry curriculum [9,20,26]. Landi, et al. [16] reported that younger than 41 years old dentists are more aware of patients undergoing anti-resorptive therapy and their clinical implications. Similar to the mentioned studies, in this study, the awareness of dentists who graduated in 2014 or later was higher than others because AAOMS updated the term BRONJ to MRONJ in 2014.
There is very limited data describing the occurrence of MRONJ in the pediatric population for osteogenesis imperfecta and other conditions. In a systematic review estimating the risk of MRONJ among children with osteogenesis imperfecta, there were no cases of MRONJ identified in a sample of 486 subjects treated for 4.5 to 6.8 years [27]. In a different study that estimated the risk for MRONJ among those under the age of 24, no cases were reported [28]. Since dentists who deal with a young patient profile such as (eg. Pedodontists, Orthodontists) and mostly deal with dental hard tissue (eg. Endodontists, Restorative dentists) are less likely to encounter MRONJ, their awareness and knowledge levels also changeable as shown in this study.
Al Samman & Al Ani [8] studied a group consisting of 113 GDP, 33 OMR, and 32 OMS. A significant difference existed among the groups with a rate of MRONJ’s awareness of 34%, 49%, and 84% for GDP, OMR, and OMS respectively. Concerning MRONJ knowledge, significantly higher rates were seen in the OMS set with a score of 49%. In contrast, the score for OMR was 31%, and the GDP group had the lowest score of 17%. Aslan, et al. [12] revealed in their study that OMR and OMS were able to achieve higher correct answer rates than other dental specialties. (p > 0.05). In accordance with Aslan et al.’s study, we found that OMRs and OMS have higher awareness of MRONJ than other specialties. This may be because they are the specialists who usually encounter these patients and drugs. This can be explained by the fact that MRONJ patients are encountered more frequently in university dental hospitals [29], and the mentioned specialties particularly have more experience with such patients [12].
Some studies reported that OMS is more knowledgeable about MRONJ [26,29-31]. The reason for mentioning only OMS regarding the high level of MRONJ knowledge in the previous questionnaires may be the absence [26,29,31] or the small number [32] of OMS in such studies.
Although several surveys including dental students, GDP, OMS, prescribers, and patients, were carried out in different geographical areas, in an attempt to identify the level of knowledge, awareness, and clinical experience about MRONJ [7-11], there are only a few investigations involving dental specialists among participants [12,13,32]. Therefore, this is a rare study evaluating the awareness and knowledge of dentists according to their graduation and specialization.
Limitations
This study was conducted as part of the graduation project at Ondokuzmayıs University, Faculty of Dentistry in 2023-2024. This is because, the online questionnaire was designed by three senior students, with no experience, but under the supervision of an OMR with 20 years of experience.
The questionnaire in the present study was conducted based on the 2014 position paper of AAOMS [5]. Recently, the AAOMS released a 2022 update that includes changes in MRONJ definition criteria, medications, and management strategies [26]. In this study, participants were asked about the 2014 definition of MRONJ because there were a few graduated dentists who received 2022 updated dental education.
Also, the ST group consists of specialists and specialty trainers because of the smaller number of participants, and this group showed a non-homogeneous distribution for each specialty/doctoral program.
According to our knowledge, there is no study comparing dentists’ graduation date in terms of being aware of MRONJ coined in 2014 in the literature. In this study, it was seen that dentists who graduated in 2014 or later were better, as we expected, due to MRONJ being termed in the literature in 2014 and entering the dentistry education curriculum after that. In addition, the awareness and knowledge of ST were higher than GDP, during specialist training, which may be because they experienced these cases more. Furthermore, awareness and knowledge of OMR and OMS were higher which may be because during specialist training, they were informed more about this subject, and also, they encounter these patients more frequently in their career.
The authors of this study suggest that more studies involving a high and similar number of participants from all dental specialties and speciality trainers may be helpful to determine the actual knowledge levels of different specialties.
In our opinion, planning educational strategies for all dentists, especially GDP and dentists who graduated before 2014, is very important. Also, the undergraduate and postgraduate dental education system should be revised in light of current information on MRONJ.
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: A growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–7. Available from: https://doi.org/10.1016/s0278-2391(03)00720-1
- Pazdur R. Postmarketing safety review: Bisphosphonates. Food and Drug Administration, Office of Drug Safety.
- Bisphosphonates and other drugs affecting bone metabolism. In: British National Formulary. 69th ed. 2014;513.
- Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J Oral Maxillofac Surg. 2009;67(5 Suppl):2-12. Available from: https://doi.org/10.1016/j.joms.2009.01.009
- Ruggiero SL, Dodson TB, Fantasia J; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72(10):1938-1956. Available from: https://doi.org/10.1016/j.joms.2014.04.031
- Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. American Association of Oral and Maxillofacial Surgeons' Position Paper on Medication-Related Osteonecrosis of the Jaws-2022 Update. J Oral Maxillofac Surg. 2022;80(5):920-943. Available from: https://doi.org/10.1016/j.joms.2022.02.008
- Al-Eid R, Alduwayan T, Bin Khuthaylah M, Al Shemali M. Dentists' knowledge about medication-related osteonecrosis of the jaw and its management. Heliyon. 2020;6(7). Available from: https://doi.org/10.1016/j.heliyon.2020.e04321
- Al-Samman AA, Al-Ani RS. A cross-sectional survey on medication-related osteonecrosis of the jaws' knowledge and awareness in a sample of dental society. J Cranio-Maxillofac Surg. 2019;47(6):926–931. Available from: https://doi.org/10.1016/j.jcms.2019.02.006
- Escovedo M, García-Consuegra L, Junquera S, Olay S, Ascani G, Junquera L. Medication-related osteonecrosis of the jaw: A survey of knowledge, attitudes, and practices among dentists in the principality of Asturias (Spain). J Stomatol Oral Maxillofac Surg. 2018;119(5):395-400. Available from: https://doi.org/10.1016/j.jormas.2018.04.008
- Levin CK, Baker J, Nolan P, Coffey A. A survey of medication-related osteonecrosis of the jaw reporting and risk assessment by oral and maxillofacial surgeons. J Oral Maxillofac Surg. 2020;78(10)-E91. Available from: https://www.joms.org/article/S0278-2391(20)30931-9/abstract
- Tanna N, Steel C, Stagnell S, Bailey E. Awareness of medication-related osteonecrosis of the jaws (MRONJ) amongst general dental practitioners. Br Dent J. 2017;222(2):121-125. Available from: https://doi.org/10.1038/sj.bdj.2017.79
- Aslan E, Sener E, Önem E, Mert A, Çankaya H. Postgraduate dental students’ knowledge levels toward medication-related osteonecrosis of the jaws. Clin Exp Health Sci. 2023;13:829-836. Available from: https://doi.org/10.33808/clinexphealthsci.1209004
- Patil V, Acharya S, Vineetha R, Nikhil K. Awareness about medication-related osteonecrosis of the jaw among dental professionals: A multicenter study. Oral Health Prev Dent. 2020;18:505-509. Available from: https://doi.org/10.3290/j.ohpd.a43361
- Acharya S, Patil V, Ravindranath V, Kudva A, Nikhil K. Medication-related osteonecrosis of the jaw: Knowledge and perceptions of medical professionals on the usage of bone modifying agents and dental referrals. J Med Life. 2022;15(3):368-373. Available from: https://doi.org/10.25122/jml-2021-0085
- Ekici Ö. Awareness of medication-related osteonecrosis of the jaw among dentists working at public oral and dental health care centers in Ankara, Turkey. Turkiye Klinikleri J Dental Sci. 2021;27(1):98-107. Available from: http://dx.doi.org/10.5336/dentalsci.2020-74342
- Landi L, Oteri G, Barbato L, Discepoli N, Carrassi AM, Rigoni M, et al. Anti-resorptive therapy and MRONJ: A survey of the Italian Society of Periodontology and Implantology. Oral Dis. 2024. Available from: https://doi.org/10.1186/s10195-023-00713-7
- Saad F, Brown JE, Van Poznak C, Ibrahim T, Stemmer SM, Stopeck AT, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: Integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23:1341. Available from: https://doi.org/10.1093/annonc/mdr435
- Yamazaki T, Yamori M, Ishizaki T, Asai K, Goto K, Takahashi K, et al. Increased incidence of osteonecrosis of the jaw after tooth extraction in patients treated with bisphosphonates: A cohort study. Int J Oral Maxillofac Surg. 2012;41:1397. Available from: https://doi.org/10.1016/j.ijom.2012.06.020
- Vahtsevanos K, Kyrgidis A, Verrou E, Katodritou E, Triaridis S, Andreadis CG, et al. Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol. 2009;27:5356. Available from: https://doi.org/10.1200/jco.2009.21.9584
- Arnaud MP, Talibi S, Lejeune-Cairon S. Knowledge and attitudes of French dentists on bone resorption inhibitors (bisphosphonates and denosumab): A cross-sectional study. J Stomatol Oral Maxillofac Surg. 2022;123(2):163-170. Available from: https://doi.org/10.1016/j.jormas.2021.04.010
- Nicolatou-Galitis O, Schiødt M, Mendes RA, Ripamonti C, Hope S, Drudge-Coates L, et al. Medication-related osteonecrosis of the jaw: Definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127:117-135. Available from: https://doi.org/10.1016/j.oooo.2018.09.008
- Hallmer F, Andersson G, Gotrick B, Warfvinge G, Anderud J, Bjørnland T. Prevalence, initiating factor, and treatment outcome of medication-related osteonecrosis of the jaw—a 4-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126:477. Available from: https://doi.org/10.1016/j.oooo.2018.08.015
- Sturrock A, Preshaw PM, Hayes C, Wilkes S. Perceptions and attitudes of patients towards medication-related osteonecrosis of the jaw (MRONJ): A qualitative study in England. BMJ Open. 2019;9(3). Available from: https://doi.org/10.1136/bmjopen-2018-024376
- British Dental Association. The state of general dental practice in 2013. Accessed January 2017.
- Ekmekcioglu A, Akay G, Karadag O, Gungor K. The awareness and knowledge of dentists of medication-related osteonecrosis of the jaw. Clin Exp Health Sci. 2021;11:163-169. Available from: https://dergipark.org.tr/en/download/article-file/999751
- Alhussain A, Peel S, Dempster L, Clokie C, Azarpazhooh A. Knowledge, practices, and opinions of Ontario dentists when treating patients receiving bisphosphonates. J Oral Maxillofac Surg. 2015;73(6):1095-1105. Available from: https://doi.org/10.1016/j.joms.2014.12.040
- Hennedige AA, Jayasinghe J, Khajeh J, Macfarlane TV. Systematic review on the incidence of bisphosphonate-related osteonecrosis of the jaw in children diagnosed with osteogenesis imperfecta. J Oral Maxillofac Res. 2013;4. Available from: https://doi.org/10.5037/jomr.2013.4401
- Duarte NT, Rech BO, Martins IG, Franco JB, Ortega KL. Can children be affected by bisphosphonate-related osteonecrosis of the jaw? A systematic review. Int J Oral Maxillofac Surg. 2020;49:183. Available from: https://doi.org/10.1016/j.ijom.2019.08.004
- Yoo JY, Park YD, Kwon YD. Survey of Korean dentists on the awareness of bisphosphonate-related osteonecrosis of the jaws: A survey on the awareness of BRONJ. J Investig Clin Dent. 2010;1(2):90-95. Available from: https://doi.org/10.1111/j.2041-1626.2010.00024.x
- Sahin O. Medication-related osteonecrosis of the jaw: A survey of knowledge, practices, and opinions of dentists. Ann Med Res. 2020;27(9):2421-2427. Available from: https://annalsmedres.org/index.php/aomr/article/view/932
- Gaballah K, Hassan M. Knowledge and attitude of dentists on bisphosphonates use in the UAE: A descriptive cross-sectional study. Int Surg J. 2017;4(4):1398. Available from: https://doi.org/10.18203/2349-2902.isj20171150
- Deveci H, Ugar Cankal DA. Investigation of the approach of dentists in Ankara to patients who use drugs such as bisphosphonates, denosumab, and similars. ADO Klinik Bilimler Dergisi. 2021;10(2):99-105. Available from: https://dergipark.org.tr/tr/download/article-file/1601489