More Information
Submitted: February 22, 2024 | Approved: April 26, 2024 | Published: April 29, 2024
How to cite this article: Azimzadeh M, Esmaeili F, Bayat N, Rahimipour K, Tolouei AE. Texture Analysis of Hard Tissue Changes after Sinus Lift Surgery with Allograft and Xenograft. J Oral Health Craniofac Sci. 2024; 9: 019-022.
DOI: 10.29328/journal.johcs.1001049
Copyright License: © 2024 Azimzadeh M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Diagnostic imaging; Texture analysis; Maxillary sinus; Allografts; Xenografts
Abbreviations: CBCT: Cone Beam Computed Tomography; TA: Texture Analysis
Texture Analysis of Hard Tissue Changes after Sinus Lift Surgery with Allograft and Xenograft
Mohammad Azimzadeh1, Farzad Esmaeili2, Narges Bayat2, Kasra Rahimipour3 and Amir Ebrahimpour Tolouei1*
1DDS, Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
2Associate Professor, Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
3DDS, Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
*Address for Correspondence: Amir Ebrahimpour Tolouei, DDS, Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran, Email: [email protected]
In the realm of dental surgery, implants are essential for replacing missing teeth. To facilitate implant placement, techniques such as bone grafting and sinus lifts are utilized to augment the volume of atrophied alveolar bone in candidates for dental implants. Typically, patients undergo a period of recovery following bone grafts before proceeding with implant placement. This study investigates the efficacy of Cone Beam Computed Tomography (CBCT) in measuring the residual bone volume and assessing bone quality after the healing phase. A texture analysis was conducted on CBCT scans from 42 patients requiring maxillary sinus lift reconstruction. These patients were categorized into two groups based on the type of grafting material used: Xenograft or allograft. The study analyzed the distribution of various texture parameters and conducted a Mann-Whitney U test to identify significant statistical differences between the groups. Results indicated non-normal distributions for specific variables such as Area_S(1,0) and S(1,0)SumOfSqs, while others like S(1,0)Entropy displayed normal distributions. The findings revealed no significant statistical differences in the primary outcomes between the xenograft and allograft groups. However, the average values of the gray shades of pixels in the allograft group were statistically significantly higher compared to the xenograft group, suggesting differences in bone texture post-procedure.
Replacing missing teeth has historically been a challenge in dental medicine. For decades, removable dentures were the standard solution, offering a simple but often uncomfortable option for patients due to the mobility of these prostheses. With the advent of dental implants, a more stable and fixed prosthesis became available, significantly reducing discomfort associated with traditional dentures. However, implant stabilization remains particularly challenging in the posterior areas of the upper jaw, where limited bone volume and proximity to the sinus can complicate procedures [1]. Sinus pneumatization following tooth extraction often leads to alveolar bone atrophy, further exacerbating the loss of suitable implant sites [2,3].
Although recent studies suggest that short implants may be effective in areas with reduced bone volume [4,5], sinus bone augmentation has proven to be a reliable method for enhancing implant anchorage. This technique involves the careful elevation of the Schneiderian membrane to avoid perforation and the placement of bone graft material into the newly created space above the sinus [4,6]. Depending on the height of the remaining alveolar bone, implants may be placed simultaneously with bone grafts if sufficient primary stability can be achieved.
Cone Beam Computed Tomography (CBCT) has emerged as a critical tool in this context, enabling precise measurement of residual bone and assessment of the graft site post-procedure [7-10]. This study aims to evaluate the effectiveness of sinus lift augmentations using two different types of graft materials: xenografts and allografts. By examining the transplanted areas and analyzing the outcomes, this research seeks to enhance our understanding of the comparative benefits of these materials in promoting successful dental implantation, thus guiding future clinical practices.
This study was conducted in accordance with the World Medical Association Declaration of Helsinki (of 1975 as revised in 2000) and was approved by the ethics committee of Tabriz University of Medical Sciences. (Institutional Review Board: IR.TBZMED.REC.1400.1023).
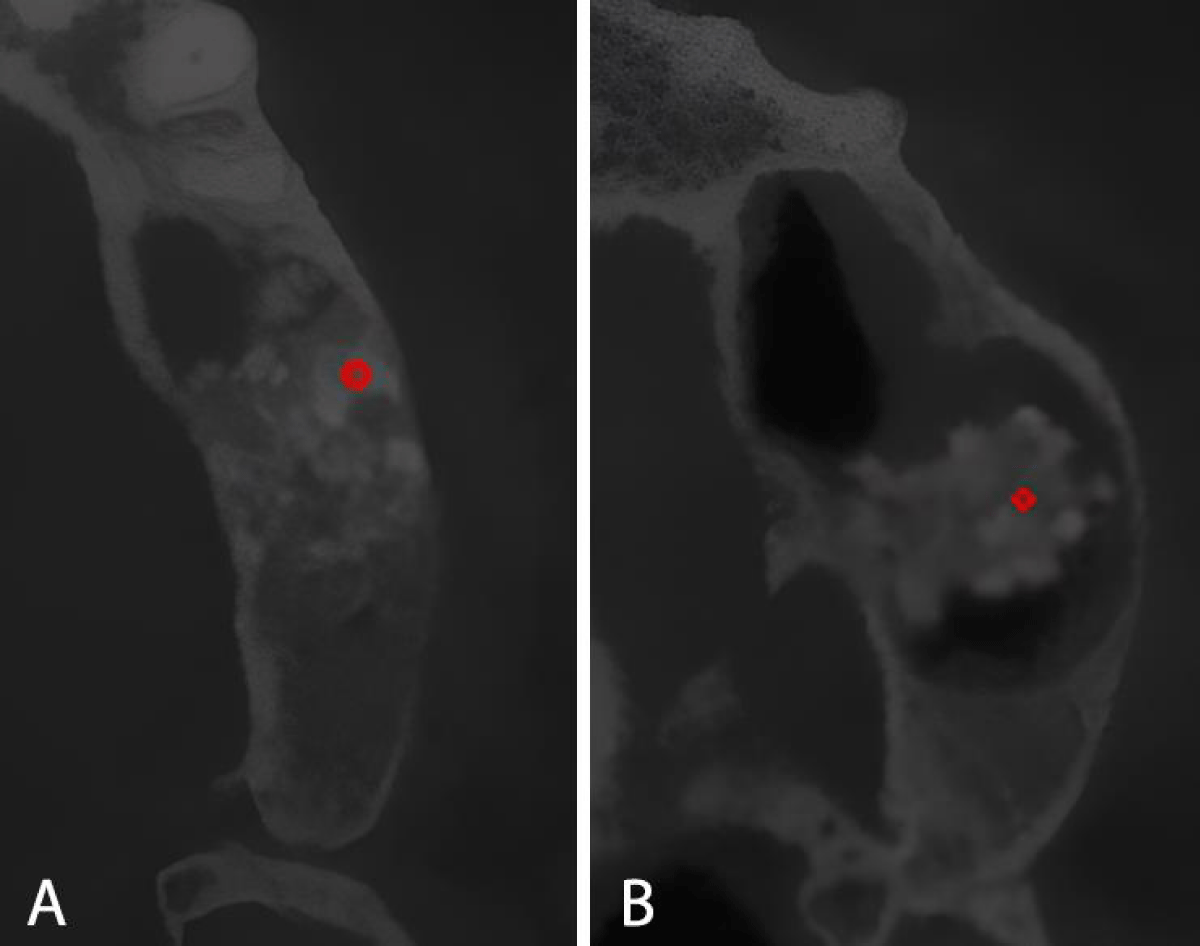
42 patients with bone loss in the posterior region of the upper jaw were selected for the sinus lift procedure. CBCT images were divided into 2 categories; using xenograft or allograft material. Texture analysis (TA) was done by MaZda Software (Technical University of Lodz, Institute of Electronics, Poland) on the images obtained in the axial sections (Figure 1). Transplantation was done in all patients by one surgeon using the same protocol. CBCT scans were performed with a Newton 3D scanner (VGI, QR SRL, made in Italy) at the Faculty of Dentistry, Tabriz University of Medical Sciences. Then, all CBCT images were used for DICOM analysis, and images containing artifacts that reduce resolution (such as beam hardening artifacts, partial volume effect, aliasing artifacts, ring artifacts, etc.) were removed. Then the desired ROI will be selected at the center of the examined area of the bone graft sites to evaluate the grey-level co-occurrence Matrix (GLCM). Eleven texture parameters, listed in Table 1, were extracted for each ROI on each slice [11].
Figure 1: Example of ROI measurements in 2 different groups (A. Allograft, B.Xenograft).
| Table 1: Texture parameters used in the analysis. | |
| Texture parameter | Description |
| Contrast | Represents the amount of local variation of gray shades |
| Inverse difference moment (InvDfMom) | Homogeneity of the distribution of gray shades on the image |
| Angular second moment (AngScMom) | Measurement of image uniformity |
| Correlation | Linear measure dependence of gray shades between neighboring pixels |
| Sum of squares | Measurement of the dispersion (related to average) of gray shade distribution |
| Entropy | Degree of disorder between pixels in the image |
| Sum of average | Mean of the distribution of the sum of gray shades |
| Sum of variance (SumVarnc) | Dispersion around the mean of the sum distribution of gray shades |
| Sum of entropy (SumEntrp) | Disorganization of the sum distribution of gray shades |
| Difference of variance | Dispersion of the gray shade difference |
| Difference of entropy | Disorganization of the gray shade difference |
GLCM is a square matrix that can show certain features about the spatial resolution of the image. A statistical method is used which is calculated through the distribution of gray shades and it is related to the number of times the amount of gray shade in dimensions i and j of the two-dimensional matrix of the image are equal in the 1-, 2-, 3-, 4- and 5-pixel intervals and at specific angles (0-45-90 and 135 degrees). Finally, the results obtained from the software will be used to compare the contrast, homogeneity, and texture complexity of hard tissue in the three different groups. With the help of the parameters obtained from this technique, it is possible to obtain the average gray levels and the way pixels change, which has the highest diagnostic value in examining healthy and pathological tissue changes [11].
The normality of distribution for our data was assessed using the Kolmogorov-Smirnov test, a non-parametric method suitable for samples of any size. This test was conducted using IBM SPSS software (version 23; IBM Inc., Armonk NY, USA). The timeframe of the study spanned from 2022 to 2023, utilizing current CBCT technology and methodologies.
The Kolmogorov-Smirnov test was used to check the normal distribution of the variables. The test’s significance level, detailed in Table 2, was established at 0.05. Table 2 presents an analysis of eleven factors relating to the selection of texture parameters and their statistical significance across different groups. The results posit that:
| Table 2: Texture parameters selection and statistical significance for groups (p < 0.05). | |||||
| Variable | Group | N | Mean | Std. Deviation | p value |
| S(1,0)AngScMom | xenograft | 21 | 0.2749 | 0.13919 | 0.772 |
| Allograft | 21 | 0.2868 | 0.12648 | ||
| S(1,0)Contrast | xenograft | 21 | 0.391 | 0.17267 | 0.565 |
| Allograft | 21 | 0.3609 | 0.1633 | ||
| S(1,0)Correlat | xenograft | 21 | 0.5383 | 0.19794 | 0.715 |
| Allograft | 21 | 0.5586 | 0.15782 | ||
| S(1,0)InvDfMom | Xenograft | 21 | 0.8084 | 0.08822 | 0.431 |
| Allograft | 21 | 0.827 | 0.06092 | ||
| S(1,0)SumAverg | Xenograft | 21 | 15.9486 | 1.29069 | < 0.001 |
| Allograft | 21 | 18.8017 | 1.34378 | ||
| S(1,0)SumVarnc | Xenograft | 21 | 1.7154 | 1.19312 | 0.426 |
| Allograft | 21 | 1.4572 | 0.85861 | ||
| S(1,0)SumEntrp | Xenograft | 21 | 0.6161 | 0.1651 | 0.6 |
| Allograft | 21 | 0.5922 | 0.12472 | ||
| S(1,0)Entropy | Xenograft | 21 | 0.7321 | 0.20768 | 0.604 |
| Allograft | 21 | 0.7021 | 0.16138 | ||
A) There was no clear statistical difference between the means of variables S(1,0)AngScMom, S(1,0)Contrast, S(1,0)Correlat, S(1,0)InvDfMom, S(1,0)SumVarnc, S(1,0) 0) (SumEntrp and S(1,0)Entropy) in the two investigated groups (p > 0.05).
B) There was a clear statistical difference between the means of variable S(1,0)SumAverg in the two investigated groups, and the means mentioned in the allograft group were higher than the xenograft group (p < 0.05).
The nature of the materials used in sinus augmentation has evolved in the past decades: initially, autograft was the only possible way for the procedure, which was taken from the ilium, tibia, or chin bone [12-17]. Cortical bone grafting was used for the upper parts of the sinus and trabecular bone grafting was used for the lower parts of the sinus cavity for augmentation. Currently, the complications of autografted bone are well-defined. In this case, the volume of bone autograft to be removed is moderate, and other limitations such as increased morbidity and limited availability are related to it [18]. On the other hand, xenografts and allografts are alternatives with less morbidity rate which eliminate the need for a secondary surgical (donor) site [4,19].
Previous studies on TA such as what Ditmer, et al. performed demonstrated the ability of TA to differentiate tissues Based on the characteristics between lesions of a tumor (high and low-grade tumors), including quantifying changes in surface characteristics [20].
The application of TA is a useful technique to differentiate between normal and abnormal tissues. All these parameters are suitable to characterize the gray-level distribution of regions of interest (ROIs) and accentuate features from images that have usually been missed by the human eye [21,22].
This method can be used to measure the quality of bone in the transplanted areas to determine the radiographic features when the gross structure has completely disappeared.
Our study confirms that texture analysis (TA) of Cone Beam Computed Tomography (CBCT) images effectively evaluates areas augmented with allograft and xenograft materials. Although there were no significant statistical differences between the two groups for most parameters, we observed that the distribution of gray shades of pixels was significantly higher in the allograft group compared to the xenograft group. This finding suggests that allografts may influence bone texture more distinctly, a consideration that could guide material selection in clinical practice.
Ethical approval
This study was conducted in accordance with the World Medical Association Declaration of Helsinki (of 1975 as revised in 2000) and was approved by the ethics committee of Tabriz University of Medical Sciences. (Institutional Review Board: IR.TBZMED.REC.1400.1023).
- Block MS, Kent JN. Maxillary sinus grafting for totally and partially edentulous patients. J Am Dent Assoc. 1993 May;124(5):139-43. doi: 10.14219/jada.archive.1993.0127. PMID: 8482771.
- Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology--eleven years of surgical experience (1979-1990). J Oral Implantol. 1990;16(3):199-209. PMID: 2098563.
- Del Fabbro M, Testori T, Francetti L, Weinstein R. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004 Dec;24(6):565-77. PMID: 15626319.
- Froum SJ, Tarnow DP, Wallace SS, Rohrer MD, Cho SC. Sinus floor elevation using anorganic bovine bone matrix (OsteoGraf/N) with and without autogenous bone: a clinical, histologic, radiographic, and histomorphometric analysis--Part 2 of an ongoing prospective study. Int J Periodontics Restorative Dent. 1998 Dec;18(6):528-43. PMID: 10321168.
- Hockers T, Abensur D, Valentini P, Legrand R, Hammerle CH. The combined use of bioresorbable membranes and xenografts or autografts in the treatment of bone defects around implants. A study in beagle dogs. Clin Oral Implants Res. 1999 Dec;10(6):487-98. doi: 10.1034/j.1600-0501.1999.100607.x. PMID: 10740458.
- Tadjoedin ES, de Lange GL, Holzmann PJ, Kulper L, Burger EH. Histological observations on biopsies harvested following sinus floor elevation using a bioactive glass material of narrow size range. Clin Oral Implants Res. 2000 Aug;11(4):334-44. doi: 10.1034/j.1600-0501.2000.011004334.x. PMID: 11168226.
- Scarano A, Degidi M, Iezzi G, Pecora G, Piattelli M, Orsini G, Caputi S, Perrotti V, Mangano C, Piattelli A. Maxillary sinus augmentation with different biomaterials: a comparative histologic and histomorphometric study in man. Implant Dent. 2006 Jun;15(2):197-207. doi: 10.1097/01.id.0000220120.54308.f3. PMID: 16766904.
- Hatano N, Shimizu Y, Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res. 2004 Jun;15(3):339-45. doi: 10.1111/j.1600-0501.2004.00996.x. PMID: 15142097.
- Kim YK, Kim SG, Lee BG. Bone graft and implant. Narae, Seoul, Korea. 2007; 169-261.
- Graziani F, Ducci F, Tonelli M, El Askary AS, Monier M, Gabriele M. Maxillary sinus augmentation with platelet-rich plasma and fibrinogen cryoprecipitate: a tomographic pilot study. Implant Dent. 2005 Mar;14(1):63-9. doi: 10.1097/01.id.0000156387.35521.bf. PMID: 15764947.
- Gonçalves BC, de Araújo EC, Nussi AD, Bechara N, Sarmento D, Oliveira MS, Santamaria MP, Costa ALF, Lopes S. Texture analysis of cone-beam computed tomography images assists the detection of furcal lesion. J Periodontol. 2020 Sep;91(9):1159-1166. doi: 10.1002/JPER.19-0477. Epub 2020 Feb 26. PMID: 32003465.
- Wannfors K, Johansson B, Hallman M, Strandkvist T. A prospective randomized study of 1- and 2-stage sinus inlay bone grafts: 1-year follow-up. Int J Oral Maxillofac Implants. 2000 Sep-Oct;15(5):625-32. PMID: 11055129.
- Galindo-Moreno P, Avila G, Fernández-Barbero JE, Aguilar M, Sánchez-Fernández E, Cutando A, Wang HL. Evaluation of sinus floor elevation using a composite bone graft mixture. Clin Oral Implants Res. 2007 Jun;18(3):376-82. doi: 10.1111/j.1600-0501.2007.01337.x. Epub 2007 Mar 12. PMID: 17355356.
- Herzberg R, Dolev E, Schwartz-Arad D. Implant marginal bone loss in maxillary sinus grafts. Int J Oral Maxillofac Implants. 2006 Jan-Feb;21(1):103-10. PMID: 16519188.
- Rodoni LR, Glauser R, Feloutzis A, Hämmerle CH. Implants in the posterior maxilla: a comparative clinical and radiologic study. Int J Oral Maxillofac Implants. 2005 Mar-Apr;20(2):231-7. PMID: 15839116.
- Simion M, Trisi P, Piattelli A. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int J Periodontics Restorative Dent. 1994 Dec;14(6):496-511. PMID: 7751115.
- Hallman M, Zetterqvist L. A 5-year prospective follow-up study of implant-supported fixed prostheses in patients subjected to maxillary sinus floor augmentation with an 80:20 mixture of bovine hydroxyapatite and autogenous bone. Clin Implant Dent Relat Res. 2004;6(2):82-9. doi: 10.1111/j.1708-8208.2004.tb00030.x. PMID: 15669708.
- Danesh-Sani SA, Loomer PM, Wallace SS. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Br J Oral Maxillofac Surg. 2016 Sep;54(7):724-30. doi: 10.1016/j.bjoms.2016.05.008. Epub 2016 May 25. PMID: 27235382.
- Oklund SA, Prolo DJ, Gutierrez RV, King SE. Quantitative comparisons of healing in cranial fresh autografts, frozen autografts and processed autografts, and allografts in canine skull defects. Clin Orthop Relat Res. 1986 Apr;(205):269-91. PMID: 3516501.
- Ditmer A, Zhang B, Shujaat T, Pavlina A, Luibrand N, Gaskill-Shipley M, Vagal A. Diagnostic accuracy of MRI texture analysis for grading gliomas. J Neurooncol. 2018 Dec;140(3):583-589. doi: 10.1007/s11060-018-2984-4. Epub 2018 Aug 25. PMID: 30145731.
- Oliveira MS, Fernandes PT, Avelar WM, Santos SL, Castellano G, Li LM. Texture analysis of computed tomography images of acute ischemic stroke patients. Braz J Med Biol Res. 2009 Nov;42(11):1076-9. doi: 10.1590/s0100-879x2009005000034. Epub 2009 Oct 9. PMID: 19820884.
- Ramkumar S, Ranjbar S, Ning S, Lal D, Zwart CM, Wood CP, Weindling SM, Wu T, Mitchell JR, Li J, Hoxworth JM. MRI-Based Texture Analysis to Differentiate Sinonasal Squamous Cell Carcinoma from Inverted Papilloma. AJNR Am J Neuroradiol. 2017 May;38(5):1019-1025. doi: 10.3174/ajnr.A5106. Epub 2017 Mar 2. PMID: 28255033; PMCID: PMC7960372.