More Information
Submitted: January 08, 2024 | Approved: January 17, 2024 | Published: January 18, 2024
How to cite this article: Wänman A, Marklund S, Yekkalam N. Treatment Outcome in Patients with Myofascial Orofacial Pain. A Randomized Clinical Trial. J Oral Health Craniofac Sci. 2024; 8: 001-008.
DOI: 10.29328/journal.johcs.1001046
Copyright License: © 2024 Wänman A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Oral appliance; Exercise; Myalgia; Physiotherapy; Temporomandibular disorders
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial
Anders Wänman*, Susanna Marklund and Negin Yekkalam
Department of Odontology, Clinical Oral Physiology, Umeå University, Umeå, Sweden
*Address for Correspondence: Anders Wänman, Professor, Department of Odontology, Clinical Oral Physiology, Umeå University, Umeå, Sweden, Email: [email protected]
Background: Temporomandibular Disorder (TMD) pain attributed to myalgia is a common condition and patients should get advice on the best treatment option.
Objectives: The aim was to evaluate the effect of two different exercise programs, or bite splint therapy, respectively, in patients with chronic frequent primary myofascial orofacial pain.
Methods: The study was a randomized clinical trial including patients fulfilling criteria of chronic frequent primary myofascial orofacial pain with a reported pain intensity of ≥ 4 on a numerical rating scale (0-10). Ninety subjects were randomized to either bite splint, home exercises, or a supervised exercise program. Two examiners blinded to the treatment modality examined the same subject at baseline and a 3-month follow-up. Non-parametric statistical methods were applied for the outcome of treatment in intended-to-treat analyses. A P-value <0.05 was considered statistically significant.
Results: The pain severity index was significantly reduced (p < 0.001) in all treatment groups. Jaw opening capacity improved significantly (p < 0.05) for those randomized to bite splint and for those in the home exercise program. About 70% of the participants reported improvement in their TMD pain severity with no significant difference between treatments. Both exercise groups improved in jaw function at the 3-month follow-up compared to baseline. Those who had a bite splint reported significantly more improvement in their headaches compared to those in the exercise programs.
Conclusion: Jaw exercise programs and bite splint treatments had similar positive effects on TMD pain severity attributed to myalgia after 3 months.
Temporomandibular Disorders (TMD) include symptoms such as pain around the temporomandibular joint and jaw muscles, pain in jaw movements, impaired jaw mobility, and temporary or persistent locking of the jaw [1]. These symptoms are common in the population and negatively affect the individual’s oral health and general well-being [2,3]. The treatment needed owing to TMD is estimated within the range of 5% to 20% [4]. Dentists are thus expected to frequently meet and manage patients with TMD of varying severity in their daily practice. Different conservative treatment modalities are recommended for patients with TMD. These include advice, dental splints, jaw exercises, and over-the-counter medication. The treatment regimens may also involve costlier, resource-demanding, and irreversible therapies such as orthodontics, prosthodontics, and surgery.
Best practice of patients with TMD was one of the main topics when the Swedish National Board of Health and Welfare generated National Guidelines for Dental Health Care in Sweden [5]. The review clearly revealed that robust science based on randomized clinical studies of high quality was generally lacking, which consequently has an impact on clinical decision-making. Published studies on the effect of physiotherapy/exercises on TMD can be divided into those mainly focusing on correction of head and mandible position and those including stretching exercises of the jaw, with or without combination with other treatment modalities [6]. Although the studies indicate a beneficial effect, they are heterogeneous in terms of study populations, diagnoses, treatment modalities, and outcome measures. Other drawbacks are a lack of description of intention-to-treat measures, reasons for dropouts, evaluation of patient compliance, use of rescue medication, and side effects [7]. Knowledge of the effect of activating the jaw-motor system in different specific common conditions related to TMD is generally lacking. Thus, there is a need for well-designed randomized clinical trials to improve the scientific base of knowledge of the potential benefits of introducing such treatment regimes in patients hampered by TMD.
We have previously published the outcome of a randomized clinical trial on patients with symptomatic disc displacement with reduction [8]. The patients were randomized to treatment with either a bite splint or a home-exercise program based on exercises used in a study by Au and Klineberg [9] and in a study by Yoda, et al. [10] or by exercises in a supervised exercise program [8]. The outcome was in favor of the supervised program, but all tested interventions had a positive effect on the patient’s main symptom – temporomandibular clicking sounds.
Another common diagnosis within the concept of Temporomandibular Disorder (TMD) pain is myalgia. Conservative treatment modalities, such as advice, bite splints, jaw exercises, and over-the-counter medication are recommended as primary interventions for patients with TMD pain [11,12]. We have previously in a qualitative study reported that patients with myalgia experienced a program with supervised exercise of the jaw-neck system positively as a valuable part of their rehabilitation [13].
The primary aim of this study was to evaluate the effect of supervised and home exercise programs, respectively, among patients with frequent chronic primary myofascial orofacial pain. The second aim was to evaluate if there is a significant difference in outcomes between a supervised exercise program, home exercise program, and bite splint therapy. Bite splint therapy was used as ¨standard treatment¨. The third aim was to identify possible factors associated with a less favorable treatment outcome. Our null hypothesis was that the different treatment modalities would show similar outcomes. The second hypothesis was that high depression and somatization scores would be identified as factors related to a less favorable outcome.
Study design
The study design was a blinded Randomized Controlled Clinical Trial (RCT) with three parallel treatment groups comprised of 30 subjects in each group. The participants were examined at baseline and re-examined after 3 months. The study was approved by the Regional Ethical Review Board in Umeå, Sweden, (Dnr 2011-219-31M) and carried out in accordance with the Declaration of Helsinki.
Study-population
Participants were recruited from patients referred to the Clinical Oral Physiology department in Umeå, Sweden as well as among those who responded to targeted advertising. Those who fulfilled the inclusion criteria after an examination received oral and written information about the study. Those who were willing to participate signed an informed consent. In total 593 individuals were screened, and 90 subjects were included in the trial.
The general inclusion criteria were age between 18 and 70 years, accommodation in Umeå Municipality’s proximity, and a good understanding of Swedish, both oral and written language. The exclusion criteria were the presence of a major psychiatric diagnosis, ongoing dental, medical, or physiotherapeutic treatments related to the patient´s symptoms that may interfere with the study, as well as active rheumatologic disease and any malignant disease.
To be allocated to the category chronic frequent primary myofascial orofacial pain, they should have pain in the jaw-face-temple region as their major symptom. They should fulfill the Research Diagnostic Criteria for Temporo Mandibular Disorders (RDC/TMD) for myalgia [14]. The participants should indicate the severity of the pain at ≥ 4 on a Numerical Rating Scale (NRS 0-10) the frequency of pain in the jaw-face region once a week or more [15] and a pain duration of more than 3 months. They should have no clinical signs of widespread hyperalgesia based on palpation of the neck, shoulder, thumb, arm, and calf muscles. Those who responded with pain to palpation in all of these sites were considered to have widespread hyperalgesia and thus excluded [16]. None of the participants in the previously published study based on those with symptomatic disc displacement with reduction [8] was included in this trial.
Study settings
The study was performed at the Department of Odontology, Clinical Oral Physiology at Umeå University Sweden in collaboration with the Public Dental Health Service. Two specialists in clinical oral physiology/TMD/orofacial pain performed the examinations (AW and SM). Each participant had the same examiner at baseline and at the three-month follow-up. The examiner was always blinded to the participant’s intervention. Two trained assistants were engaged in the treatments but were not involved in the examinations and evaluations.
Questionnaire
After enrolment, the participants received the Swedish version of the RDC/TMD questionnaire, supplemented with the following questions regarding Jaw function limitation scale -20 (JFLS-20) [17], Neck Disability Index (NDI), Oral health impact profile (OHIP-14) and rating of the subject’s motivation to complete the intervention on NRS 0-10.
The questionnaire was filled out at the subject’s home and brought to the clinic where subjects were randomized to intervention.
At the follow-up, the participants filled out the same questionnaire as well as the Patient’s Global Impression of Change (PGIC) [15,18].
Randomizing process and blinding
Those who fulfilled the inclusion criteria were randomized into three different treatment groups. There were 30 individuals in each group. The randomization was done with the aid of SPSS 20 (randomized numbers) before the study started. No effort was made to match the patients. When a subject fulfilled the inclusion criteria and accepted to participate, an assistant contacted the subject and assigned the participant to intervention. Each participant was carefully instructed to not disclose his/her treatment allocation to the examiner at follow-up. All treatments were performed by trained assistants who were not involved in the examination and evaluation of the respective participants. The two examiners (authors) were blinded to the subject’s intervention trial.
Intervention
A. Bite-splint: One group (25 women and 5 men, mean age 39.6 years, SD 12.5) received a resilient bite splint, 4 mm thick BIOPLAST® (Scheu Dental GmbH, Iserlohn, Germany) produced in a BIOSTAR® heat and vacuum press (Scheu Dental GmbH, Iserlohn, Germany). The bite splint was adjusted by a trained assistant to have a flat surface with occlusal contacts in the molar, premolar, and canine regions. The instruction was to use the appliance during sleep. The subject was contacted by phone after one week to check if the appliance was accepted and used. After 6 weeks the assistant checked the function of the appliance and readjusted it if needed. The patient was encouraged to continue to use the appliance.
B. Home exercise: One group (23 women and 6 men, mean age 40.1 years, SD 15.2) received a home regime of jaw exercises. One participant was excluded due to signs of generalized hyperalgesia and thus was allocated to the wrong trial. The home exercise included four workouts/day with the following content:
- Posture: instruction to keep teeth apart and to avoid a forward head posture
- Coordination: rhythmical opening and closing movements of the jaw with a pace of one open-close circle per second for 3 minutes. Thereafter 30 movements of the jaw to the right and left sides, respectively.
- Passive stretching: after a warmup of 5 minutes with heated rice or a wheat pillow to the cheek, then stretch exercises of the jaw to maximum amplitude with the aid of the fingers and instruction to hold the maximum position for 10 seconds.
Added to these instructions the participants also received a training brochure with photos of the exercises and information on frequency and exercise duration. The brochure also included a diary. After 6 weeks, the subject and the assistant checked the performance of the exercise and the diary. The patient was encouraged to continue to do the exercises daily.
C. Supervised exercise: One group (23 women and 7 men, mean age 41.6 years, SD 12.8) received a supervised exercise program that included 10 sessions of approximately 30 minutes. The 1st exercise station was a 5-minute warming up of the jaw region with a heat lamp. The 2nd station involved small rhythmical jaw opening-closing movements for 6 minutes. The 3rd and 4th exercise stations comprised rhythmical jaw opening and jaw protrusion, against resistance for 3 minutes each. The 5th station was relaxation for 12 minutes. They were instructed to avoid chewing tough and hard food and instructed to have a distance between the teeth in the upper and lower jaw.
Outcomes
The outcomes were based on the domains recommended by IMMPACT [18] and the CONSORT statement: symptoms intensity, physical functioning, emotional functioning, participant’s ratings of global improvement, adverse events, and participant’s disposition. Answers to the questionnaire and observations at the clinical examinations before the start of the trial and after 3 months, were used in the assessment of the outcomes. The frequency of jaw pain, jaw fatigue, and headaches, was stated, respectively, on a 5-graded scale (never = 0, occasionally = 1, once or twice a month = 2, once a week = 3, several times a week = 4, and daily = 5). Each symptom’s intensity was stated on NRS (0-10) that was anchored as no problem (0) on one end and maximal/ unbearable 10) on the other end. A symptom index was calculated as the product of symptom frequency and intensity (0-50). A reduction of the symptom index of less than 30% was regarded as no significant improvement. Changes in jaw function limitation scale-20, signs of depression, signs of somatisation, Neck Disability Index (NDI), and OHIP-14, were all used as outcome variables as well as the Patient Global Impression of Change (PGIC).
The clinical examination at the baseline and at the follow-up included palpation of the TMJ (registration of pain to palpation, presence of TMJ joint sounds), deviation during jaw opening, TMJ load pain, and pain elicited during jaw movement. Pain to palpation of the jaw muscles, neck and shoulder muscles, and thumb, arm, and calf muscles was registered if it elicited a palpebral reflex. The vertical and horizontal overbite was registered to the nearest millimeter. Maximal jaw movement capacity (vertical and horizontal) with and without pain was registered. Pressure pain threshold was measured as the mean value of 3 measurements over the central belly of the right-hand masseter muscle at 30kPas/sec. Endurance capacity to three isotonic tasks was registered. The tasks were to do jaw opening rhythmically against a resistance of 1,6 kilogram as long as possible, to perform jaw protrusion to the same resistance as long as possible, and to perform unilateral chewing with 3 pieces of chewing gum as long as possible. For all three tasks was a time limit set to 5 minutes. The method has been described in detail previously [19]. Changes in the maximal jaw movement capacity in mm, pressure pain thresholds over the masseter muscles, and endurance time during isotonic work against resistance were included as outcome measures.
Sample size
A power calculation based on the results by Burgess, et al. [20] revealed that 21 subjects in each subgroup would be sufficient to detect a difference when α = 0.05 and β = 0.8. With an expected drop-out of 25%, the number for each trial was decided at 30 subjects. Thus, a total of 90 subjects were registered for the trials.
Statistical methods.
Analyses were based on an intention-to-treat approach. The individual baseline data was imputed for dropouts regardless of reason. Changes were calculated as the difference between baseline data and data at the 3-month follow-up. Variables with normal distribution were analyzed with independent sample t-test, and the remaining with non-parametrical Wilcoxon for paired observations and Chi-2. Factors associated with a less favorable outcome were analyzed with logistic regression analysis. A P-value <0.05 was considered statistically significant.
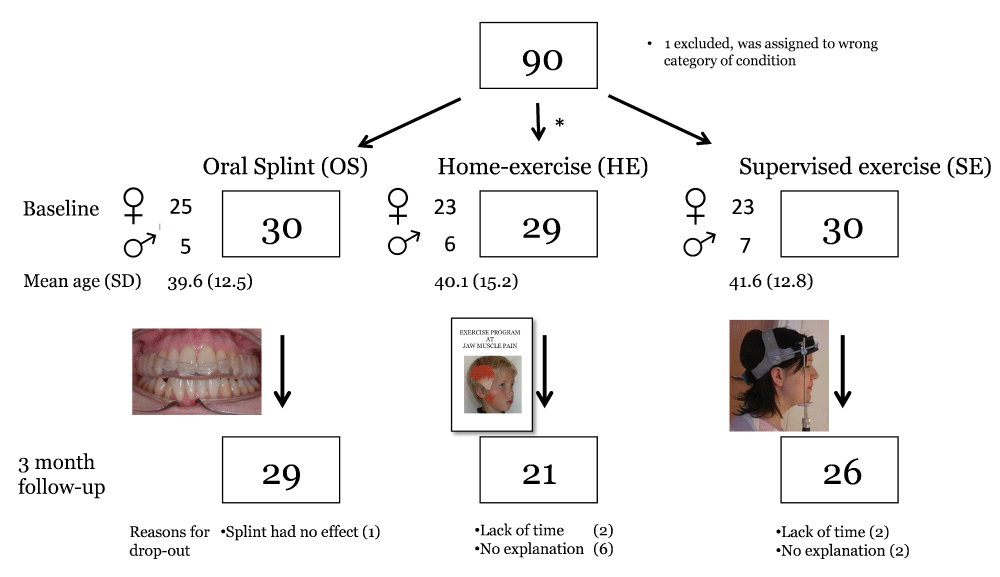
The number of participants, loss to follow-up, and reasons for dropout are presented in Figure 1. The highest number of dropouts was in the home exercise group (n = 8), compared to the bite splint group (n = 1) and supervised exercise group (n = 4). More women (n = 71) than men (n = 18) participated in the study, with no significant difference between treatment groups. The mean age of the participants was 40 years (SD 13).
Figure 1: Flowchart of randomized control trial based on patients with TMD myalgia. Gender, mean age, and reasons for dropping out were presented. One patient was assigned to the wrong category of TMD condition and thus excluded.
The mean duration of their jaw pain was 8.3 years (SD 7.3).
There were no significant gender and age differences between the treatment groups. Motivation for treatment was not significantly different (mean 8.6, SD 1.8) between the groups. The motivation was, however, significantly (p < 0.001) lower among the 13 dropouts (mean 6.9, SD 2.0) compared to those who fulfilled the treatment period until the 3-month follow-up (mean 8.8 SD 1.6).
Before treatment, the reported mean severity of jaw pain ranged from 19.9 – 23.9 on the 50-graded scale in the three treatment groups. The severity of jaw fatigue ranged from 19.4 – 22.3 and for headaches 17.0 – 22.3. The severity level was significantly reduced in all three treatment groups (post vs. pre) for these symptoms (Table 1). Depression scores and scores of OHIP-14 were also significantly reduced in all treatment groups while scores for JFLS-20 were only reduced in the exercise groups (Table 1). The mean maximal jaw opening capacity without or with pain, improved significantly in the home exercise group (Table 2). Endurance to resistance load increased significantly in both the bite-splint group and those randomized to supervised exercise (Table 2). Those in the supervised exercise group showed a significantly larger increase in endurance time compared to the other treatment groups.
| Table 1: Distribution of pre- and post-treatment values for frequent TMD symptoms, Severity of TMJ symptoms, Neck disability index (NDI), and Jaw Function Limitation Scale 20 (JFLS-20) associated to the following treatment modalities in a blinded randomized control trial: bite splint, home exercise, and supervised exercise. pre = baseline data/post = 3-month treatment follow-up data. | |||||||
| SYMPTOMS AND SYMPTOM INDICES |
Bite splint (BS) | Home exercise (HE) | Supervised exercise (SE) | Δ Pre-post | |||
| pre/post (n = 30) |
p - value¹ | pre/post (n = 29) |
p - value¹ | pre/post (n = 30) |
p - value¹ | BS: HE: SE p - value² |
|
| Jaw pain on waking up (%) | 86/60 | 0.035 | 79/69 | 83/77 | |||
| Pain in jaw, TMJ, temple (%) | 93/67 | 0.01 | 93/72 | 0.01 | 97/69 | 0.005 | |
| Pain in jaw, TMJ, temples during jaw movements (%) | 66/53 | 66/52 | 63/47 | ||||
| Severity of jaw pain (0 - 50) mean (SD) |
20.4 (10.9)/ 10.3 (10.6) |
< 0.001 | 23.9 (9.0)/ 13.6(12.4) |
< 0.001 | 19.9 (8.8)/ 10.6 (8.9) |
< 0.001 | |
| Severity of jaw fatigue (0 - 50) mean (SD) |
19.4 (14.0)/ 9.0 (10.3) |
0.003 | 22.2 (11.7)/ 15.2 (12.0) |
0.004 | 22.3 (13.9)/ 11.7 (9.6) |
< 0.001 | |
| Severity of headaches (0 - 50) mean (SD) |
22.3 (12.4)/ 10.5 (10.4) |
< 0.001 | 17.9 (11.5)/ 12.5 (10.9) |
0.01 | 17.0 (9.0)/ 12.4 (9.5) |
0.02 | BS vs. HE 0.04 BS vs. SE 0.03 |
| NDI mean (SD) |
20.3 (13.9)/ 16.6 (13.0) |
0.02 | 20.6 (12.0)/ 15.6 (11.4) |
< 0.001 | 19.7 (13.3)/ 16.9 (13.2) |
||
| Depression score mean (SD) | 0.72 (0.6)/ 0.50 (0.5) |
0.004 | 0.75 (0.8)/ 0.50(0.5) |
0.002 | 0.75 (0.7)/ 0.56 (0.6) |
0.03 | |
| Somatization score mean (SD) | 0.88 (0.6)/ 0.72 (0.5) |
0.047 | 0.91 (0.6)/ 0.62 (0.5) |
< 0.001 | 0.84 (0.6)/ 0.72 (0.5) |
||
| OHIP-14 mean (SD) |
15.2 (8.2)/ 10.1 (8.8) |
0.004 | 15.6 (8.8)/ 12.4 (7.8) |
0.002 | 13.7 (9.5)/ 10.0 (6.5) |
0.03 | |
| JFLS-20 mean (SD) |
21.1 (23.6)/ 13.9 (18.8) |
16.7 (17.8)/ 12.5 (13.1) |
0.03 | 18.2 (19.7)/ 9.7 (11.9) |
0.01 | ||
| ¹Wilcoxon’s test for paired observations, ²Independent sample t-test. | |||||||
| Table 2: Pre- and post-treatment values for registered maximal jaw mobility, associated to the following treatment modalities in a blinded randomized control trial: bite splint, home exercise, and supervised exercise. pre = baseline data/post = 3-month treatment follow-up data. | |||||||
| SIGNS | Bite splint (BS) |
Home-exercise (HE) |
Supervised exercise (SE) | Δ Pre-post | |||
| pre/post (n = 30) |
p - value¹ | pre/post (n = 29) |
p -value¹ | pre/post (n = 30) |
p -value¹ | BS: HE: SE p - value² |
|
| Jaw opening (mm) without pain mean (SD) |
41.1 (11.8)/ 45.1 (9.0) |
0.04 | 40.0 (9.4)/ 43.0 (6.2) |
0.03 | 43.5 (11.4)/ 45.8 (10.4) |
||
| Jaw opening (mm) with pain mean (SD) |
47.5 (7.8)/ 47.7 (7.3) |
44.6 (8.1)/ 47.5 (6.2) |
0.01 | 48.9 (8.1)/ 49.2 (7.0) |
HE:BS 0.048 |
||
| Pressure pain threshold Mean (SD) |
174 (55)/ 187 (69) |
170 (99)/ 188 (91) |
167 (48)/ 179 (51) |
||||
| Endurance time (sec) at isotonic jaw opening against resistance. Mean (SD) |
134 (87)/ 175 (97) |
0.006 | 172 (99)/ 176 (91) |
161 (101)/ 254 (79) |
< 0.001 | BS:HE 0.04 SE:BS 0.01 SE:HE < 0.001 |
|
| Endurance time (sec) at isotonic jaw protrusion against resistance. Mean (SD) |
150 (104)/ 177 (100) |
0.04 | 145 (117)/ 152 (93) |
139 (106)/ 245 (89) |
< 0.001 | SE:BS 0.001 SE:HE < 0.001 |
|
| Endurance time (sec) during unilateral chewing. Mean (SD) |
224 (102)/ 264 (75) |
0.004 | 239 (93)/ 263 (70) |
263 (81)/ 296 (17) |
0.03 | ||
| ¹Wilcoxon’s test for paired observations, ²Independent sample t-test. | |||||||
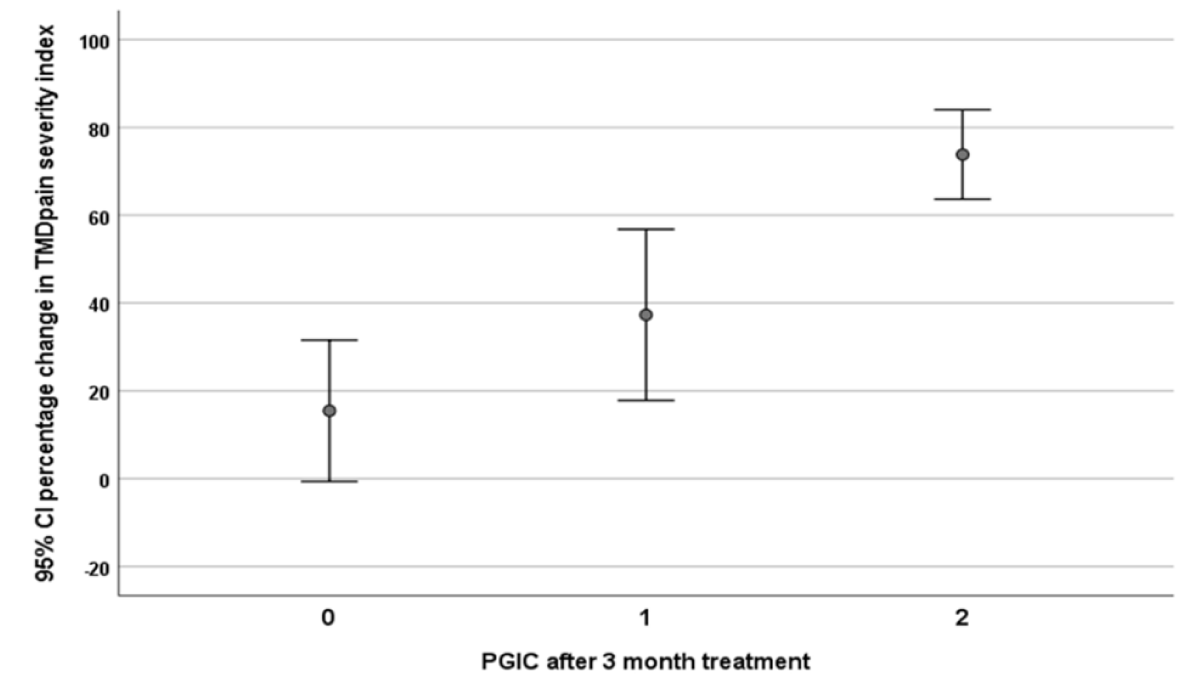
A 30% or more reduction in pain severity index was observed for 60.5% of the total sample. The relationship between the percentage change in jaw pain and PGIC is presented in Figure 2. The variables were found to be related to a pain severity index reduction of < 30% (no significant improvement). These factors were somatization score with pain (OR 2.9; 95%CI 1.28 – 6.6), somatization score without pain (OR 2.2; 95%CI 1.02 – 4.7), and dental occlusion perceived uncomfortable by the patient (OR 2.8, 95%CI 1.12 – 7.1).
Figure 2: Relationship between percentage change in TMD pain severity index after 3-month treatment and patient’s global impression of change (PGIC). O = no change; 1 = minimally improved 2 = much improved. The dashed line indicates a 30% change in TMD pain severity.
The study both revealed and confirmed some factors of importance in relation to treatment planning and decision-making in patients with chronic frequent primary myofascial orofacial pain. The outcome was favorable for the majority of the participants regardless of whether the intervention was based on an effort to reduce jaw muscle activity (bite splint therapy) or activate jaw muscles (exercise therapy). Motivation was, not surprisingly, a key to compliance. Those who were randomized to the home exercise program dropped out mostly, indicating that this would also be the outcome in the clinic. Methods should thus be developed to increase adherence to home exercise programs. The outcome of the exercise programs was related to what the patients practiced - stretching exercises improved jaw opening capacity and isotonic work against resistance improved endurance to such tasks. The jaw muscles, the TMJ, and the related connective tissues thus showed capacity to respond to the exercise applied. A less favorable outcome was related to higher somatization scores and among those who perceived that their dental occlusion was uncomfortable. These factors should thus be included in the prognosis and decision-making.
A conservative approach, including bite splint therapy, is the most commonly advocated treatment model for patients with temporomandibular disorders with an expected moderate effect on pain reduction, and a low effect on increased jaw movement capacity [21]. The present study results for bite splint therapy were in line with these results. Those who received a bite splint had an approximate 50% reduction in pain severity and an approximate 10% mean increase in jaw opening without pain. The exact mode of action for the bite splints is not known. It may reduce parafunctional activity during sleep [22] and redistribute bite force [23]. In that sense, the splint pacifies activity in jaw muscles and reduces the load on the temporomandibular joint. Resistant exercises are in principle the opposite approach since they make demands on the jaw muscles, the joint, and the associated connective tissues. Previous studies have shown that patients with TMD pain have both low bite force and endurance to both isometric and isotonic loads [19,24]. The low bite force may be related to long-term avoidance behaviours due to longstanding pain. Physiotherapy for the jaw system should thus have different targets and aims. Stretching exercises have a moderate to large effect to reduce pain and to improve jaw opening capacity [25] and in some studies even a larger effect compared to other conservative treatments for TMD [26]. In this study, similar pain reduction was reported by patients after exercises and bite splint therapy. The improvement of maximal jaw opening after home exercises, which included stretching, was less than 10% nevertheless statistically significant.
Both exercise cohorts showed improved jaw functions as evaluated based on changes in the JFLS-20 scores, however, the supervised exercise cohort improved most in endurance capacity. This indicates that the sensor-motor jaw system, although in a painful condition, is prepared to meet demands and physical challenges. The outcomes of different exercise models are the response to what is exercised. Home exercise with stretching shows improvement in maximal jaw opening capacity and the supervised program with isotonic exercises showed increased endurance and strength. In a qualitative study of supervised exercise therapy, patients experienced that they received attention and respect from the instructor. This in turn stimulated their self-efficacy and confidence resulting in better exercise effect regardless of whether the myalgia was a local condition or a part of generalized pain [13]. The long-term effects might thus differ compared to short-term outcomes.
The presence and counts of psycho-somatic symptoms, summarized in the somatization scores, affected the outcomes of the treatments even though participants with widespread pain conditions and those with signs of generalized hyperalgesia were not included in the study sample. A high somatization score, both with and without pain, affected the prognosis of conservative treatment due to TMD myalgia. Similar observations have been found previously for patients with TMD pain [27,28]. Symptoms related to depression as well as those related to neck disability did however not affect the outcomes based on the measurements used in this study. Catastrophizing thoughts have also been shown to affect treatment outcomes [29], however they were not measured in this study. In a general population-based study, those fulfilling the criteria for myalgia and arthralgia according to RDC/TMD had a higher grade of somatization (with or without pain) and depression compared to those with TMJ disc displacement, probably due to the higher pain intensity [30]. In a longitudinal multicentre study, the risk for the development of TMD pain increased among those with psychological and somatic symptoms at baseline [31]. In a cross-sectional study, higher rates of depression and somatization were mostly found among chronic TMD patients and patients with multiple TMD diagnoses [32]. Comorbidity between TMD and somatization thus seems to affect the prognosis for treatment. The practitioner should have a good knowledge of the biopsychological model to tailor TMD treatment to the individual patient.
Dental occlusion is significantly downregulated as a possible causative factor for TMD based on a lack of convincing evidence and even advocated to be abandoned in TMD practice [33]. TMD involves heterogeneous variants of conditions and comorbidities. In a population-based study were frequent jaw-face pain and headaches primarily associated with signs of regional and widespread hyperalgesia and not local pain to palpation over the masticatory muscles, central sensitization mechanisms thus seem to be involved in TMD myalgia [34]. Local biomechanical factors are not the likely causative factor in general but may still be significant in individual cases. Mandibular instability in the intercuspal position was observed as a significant factor in the development of frequent headaches [35]. The interpretation of the finding that uncomfortable fitness of dental occlusion affected the outcome of conservative treatment is hampered by the fact that the participant’s dental occlusion was not clinically assessed. The finding that the patient’s perception of an uncomfortable occlusion may be a factor to take into consideration in relation to the prognosis of the treatment planning.
The study started already year 2012 and that is the reason why the RDC/TMD criteria were used. In 2020 a new classification system was launched for pain conditions in the orofacial region – ICOP [36]. Since the patients included in this trial fulfilled the requirements for chronic frequent primary myofascial orofacial pain this term was adopted. The strength of the study was the structured procedure, regardless of which allocation the patients were randomized to, and the blinded follow-up with the same examiner. The outcome measures are well-known, established, and reliable. Since the intra-examiner variability may be lower compared to the inter-examiner variability the same examiner assessed the same patients at baseline and at follow-up. We used inclusion criteria to ensure that the pain intensity in the jaw-face region was not too mild and that the main symptom was related to myofascial pain without signs of any widespread pain condition and generalized hyperalgesia. We are thus confident that the study population represents patients with chronic frequent primary myofascial orofacial pain. One limitation of the study is that the home exercise group had a larger drop-out compared to the other two groups. Since all patients received treatment, the placebo effect was not possible to specifically estimate, but as in all types of treatment, a part of the outcome is always related to unspecified treatment effects.
Jaw exercise programs and bite splint treatments have similar positive effects on patients with chronic frequent primary myofascial orofacial pain after 3 months. Somatization and uncomfortable perception of dental occlusion were negative factors for treatment success.
Summary
Jaw exercise programs and bite splint treatments have similar positive effects on patients with chronic frequent primary myofascial orofacial pain after 3 months. Somatization and uncomfortable perception of dental occlusion were negative factors for treatment success.
A special thanks to assistants Inga-Liza Lundström and Elinor Fowler.
The study was supported by funding from The Swedish Research Council, Västerbotten County Council, and the Swedish Dental Society.
Author contribution
AW designed, and examined a part of the participants and wrote the paper. SM examined a part of the participants. All authors critically revised the manuscript.
All authors approved this version to be published and agreed to be accountable for all aspects of the work.
- Okeson JP. Etiology of functional disturbances in the masticatory system. In: Management of Temporomandibular Disorders and Occlusion. 2019.
- Qamar Z, Alghamdi AMS, Haydarah NKB, Balateef AA, Alamoudi AA, Abumismar MA, Shivakumar S, Cicciù M, Minervini G. Impact of temporomandibular disorders on oral health-related quality of life: A systematic review and meta-analysis. J Oral Rehabil. 2023 Aug;50(8):706-714. doi: 10.1111/joor.13472. Epub 2023 May 3. PMID: 37078711.
- Yekkalam N, Wänman A. Factors associated with clinical decision-making in relation to treatment need for temporomandibular disorders. Acta Odontol Scand. 2016;74(2):134-41. doi: 10.3109/00016357.2015.1063159. Epub 2015 Jul 3. PMID: 26139326.
- John MT, Reissmann DR, Schierz O, Wassell RW. Oral health-related quality of life in patients with temporomandibular disorders. J Orofac Pain. 2007 Winter;21(1):46-54. PMID: 17312641.
- National guidelines for dental care. https://www.socialstyrelsen.se/en/]
- Wänman A, Ernberg M, List T. Guidelines in the management of orofacial pain/TMD: An evidence-based approach. Tandlægebladet. 2016; 120 (3): 220-30.
- Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys Ther. 2016 Jan;96(1):9-25. doi: 10.2522/ptj.20140548. Epub 2015 Aug 20. PMID: 26294683; PMCID: PMC4706597.
- Wänman A, Marklund S. Treatment outcome of supervised exercise, home exercise and bite splint therapy, respectively, in patients with symptomatic disc displacement with reduction: A randomised clinical trial. J Oral Rehabil. 2020 Feb;47(2):143-149. doi: 10.1111/joor.12888. Epub 2019 Sep 30. PMID: 31520538; PMCID: PMC7003750.
- Au AR, Klineberg IJ. Isokinetic exercise management of temporomandibular joint clicking in young adults. J Prosthet Dent. 1993 Jul;70(1):33-9. doi: 10.1016/0022-3913(93)90034-l. PMID: 8366455.
- Yoda T, Sakamoto I, Imai H, Honma Y, Shinjo Y, Takano A, Tsukahara H, Morita S, Miyamura J, Yoda Y, Sasaki Y, Tomizuka K, Takato T. A randomized controlled trial of therapeutic exercise for clicking due to disk anterior displacement with reduction in the temporomandibular joint. Cranio. 2003 Jan;21(1):10-6. doi: 10.1080/08869634.2003.11746226. PMID: 12555926.
- Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012 Jan;143(1):47-53. doi: 10.14219/jada.archive.2012.0018. PMID: 22207667.
- De Laat A, Stappaerts K, Papy S. Counseling and physical therapy as treatment for myofascial pain of the masticatory system. J Orofac Pain. 2003 Winter;17(1):42-9. PMID: 12756930.
- Storm Mienna C, Glas L, Magnusson M, Ilgunas A, Häggman-Henrikson B, Wänman A. Patients' experiences of supervised jaw-neck exercise among patients with localized TMD pain or TMD pain associated with generalized pain. Acta Odontol Scand. 2019 Oct;77(7):495-501. doi: 10.1080/00016357.2019.1598573. Epub 2019 Apr 8. PMID: 30957601.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992 Fall;6(4):301-55. PMID: 1298767.
- Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001 Nov;94(2):149-158. doi: 10.1016/S0304-3959(01)00349-9. PMID: 11690728.
- Häggman-Henrikson B, Wiesinger B, Wänman A. The effect of supervised exercise on localized TMD pain and TMD pain associated with generalized pain. Acta Odontol Scand. 2018 Jan;76(1):6-12. doi: 10.1080/00016357.2017.1373304. Epub 2017 Sep 4. PMID: 28870137.
- Ohrbach R, Larsson P, List T. The jaw functional limitation scale: development, reliability, and validity of 8-item and 20-item versions. J Orofac Pain. 2008 Summer;22(3):219-30. PMID: 18780535.
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J; IMMPACT. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005 Jan;113(1-2):9-19. doi: 10.1016/j.pain.2004.09.012. PMID: 15621359.
- Wänman A. Endurance to physical strain in patients with temporomandibular disorders: a case-control study. Acta Odontol Scand. 2012 Dec;70(6):455-62. doi: 10.3109/00016357.2011.635599. Epub 2011 Dec 12. PMID: 22149885.
- Burgess JA, Sommers EE, Truelove EL, Dworkin SF. Short-term effect of two therapeutic methods on myofascial pain and dysfunction of the masticatory system. J Prosthet Dent. 1988 Nov;60(5):606-10. doi: 10.1016/0022-3913(88)90223-5. PMID: 3199321.
- Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS One. 2017 Feb 6;12(2):e0171296. doi: 10.1371/journal.pone.0171296. PMID: 28166255; PMCID: PMC5293221.
- Glaros AG, Owais Z, Lausten L. Reduction in parafunctional activity: a potential mechanism for the effectiveness of splint therapy. J Oral Rehabil. 2007 Feb;34(2):97-104. doi: 10.1111/j.1365-2842.2006.01660.x. PMID: 17244231.
- Gholampour S, Gholampour H, Khanmohammadi H. Finite element analysis of occlusal splint therapy in patients with bruxism. BMC Oral Health. 2019 Sep 4;19(1):205. doi: 10.1186/s12903-019-0897-z. PMID: 31484524; PMCID: PMC6727492.
- Clark GT, Beemsterboer PL, Jacobson R. The effect of sustained submaximal clenching on maximum bite force in myofascial pain dysfunction patients. J Oral Rehabil. 1984 Jul;11(4):387-91. doi: 10.1111/j.1365-2842.1984.tb00590.x. PMID: 6589384.
- Martins WR, Blasczyk JC, Aparecida Furlan de Oliveira M, Lagôa Gonçalves KF, Bonini-Rocha AC, Dugailly PM, de Oliveira RJ. Efficacy of musculoskeletal manual approach in the treatment of temporomandibular joint disorder: A systematic review with meta-analysis. Man Ther. 2016 Feb;21:10-7. doi: 10.1016/j.math.2015.06.009. Epub 2015 Jun 25. PMID: 26144684.
- Herrera-Valencia A, Ruiz-Muñoz M, Martin-Martin J, Cuesta-Vargas A, González-Sánchez M. Effcacy of Manual Therapy in TemporomandibularJoint Disorders and Its Medium-and Long-TermEffects on Pain and Maximum Mouth Opening:A Systematic Review and Meta-Analysis. J Clin Med. 2020 Oct 23;9(11):3404. doi: 10.3390/jcm9113404. PMID: 33114236; PMCID: PMC7690916.
- Jung W, Lee KE, Suh BJ. Influence of psychological factors on the prognosis of temporomandibular disorders pain. J Dent Sci. 2021 Jan;16(1):349-355. doi: 10.1016/j.jds.2020.02.007. Epub 2020 Mar 31. PMID: 33384819; PMCID: PMC7770244.
- Huttunen J, Qvintus V, Suominen AL, Sipilä K. Role of psychosocial factors on treatment outcome of temporomandibular disorders. Acta Odontol Scand. 2019 Mar;77(2):119-125. doi: 10.1080/00016357.2018.1511057. Epub 2018 Sep 28. PMID: 30264631.
- Häggman-Henrikson B, Bechara C, Pishdari B, Visscher CM, Ekberg E. Impact of Catastrophizing in Patients with Temporomandibular Disorders-A Systematic Review. J Oral Facial Pain Headache. 2020 Fall;34(4):379-397. doi: 10.11607/ofph.2637. PMID: 33290444.
- Rehm DDS, Progiante PS, Pattussi MP, Pellizzer EP, Grossi PK, Grossi ML. Depression and Somatization in Patients with Temporomandibular Disorders in a Population-Based Cross-Sectional Study in Southern Brazil. Int J Prosthodont. 2019 May/Jun;32(3):248-250. doi: 10.11607/ijp.6209. PMID: 31034538.
- Fillingim RB, Ohrbach R, Greenspan JD, Knott C, Diatchenko L, Dubner R, Bair E, Baraian C, Mack N, Slade GD, Maixner W. Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain. 2013 Dec;14(12 Suppl):T75-90. doi: 10.1016/j.jpain.2013.06.009. PMID: 24275225; PMCID: PMC3855656.
- Celić R, Braut V, Petricević N. Influence of depression and somatization on acute and chronic orofacial pain in patients with single or multiple TMD diagnoses. Coll Antropol. 2011 Sep;35(3):709-13. PMID: 22053545.
- Manfredini D, Lombardo L, Siciliani G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil. 2017 Nov;44(11):908-923. doi: 10.1111/joor.12531. Epub 2017 Jul 2. PMID: 28600812.
- Yekkalam N, Wänman A. Association between signs of hyperalgesia and reported frequent pain in jaw-face and head. Acta Odontol Scand. 2021 Apr;79(3):188-193. doi: 10.1080/00016357.2020.1814963. Epub 2020 Sep 12. PMID: 32924721.
- Marklund S, Häggman-Henrikson B, Wänman A. Risk factors associated with incidence and persistence of frequent headaches. Acta Odontol Scand. 2014 Nov;72(8):788-94. doi: 10.3109/00016357.2014.906652. Epub 2014 Apr 7. PMID: 24702010.
- International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia. 2020 Feb;40(2):129-221. doi: 10.1177/0333102419893823. PMID: 32103673.