More Information
Submitted: July 13, 2022 | Approved: July 26, 2022 | Published: July 27, 2022
How to cite this article: Robo I, Heta S, Cafaj M, Robo S, Kapaj E. Periodontal suturing, data on selection criteria. J Oral Health Craniofac Sci. 2021; 7: 010-013.
DOI: 10.29328/journal.johcs.1001038
Copyright License: © 2022 Robo I, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Suturing; Periodontal; Type of technique; Review
Periodontal suturing, data on selection criteria
Ilma Robo1*, Saimir Heta2, Migerta Cafaj3, Sonila Robo4 and Eduart Kapaj4
1Department of Therapy, Faculty of Dental Medicine, University of Medicine, Tirana, Albania
2Pediatric Surgery, Pediatric Surgeon, University Hospital Hospital, Tirana, Albania
3Department of Dentistry, Faculty of Medical Sciences, Albanian University, Tirana, Albania
4Department of Gynecology, Hospital Center, Fier, Albania
*Address for Correspondence: Ilma Robo, Department of Therapy, Faculty of Dental Medicine, University of Medicine, Tirana, Albania, Email: [email protected]
Periodontal suturing beyond the surgical elements it provides precedes the selection of the type of suture versus the fact that it is manipulated with periodontal soft tissue. This fact is the basic element in the selection of the type of suture indicated for use and the way of suturing, which in the periodontal surgeon with experience is performed instinctively without thinking.
The article is of the review type, bringing a summary of the published data about the suturing method needed for the periodontal application.
Periodontal sutures applied to the soft gingival tissues have the primary function of indication of use, the approximation of edges of the wound, the approximation of tissue boundaries where the primary healing will begin, and the proper positioning of the tissue. Beyond functionality, the surgeon must also consider aesthetic principles for high clinical outcomes. Closure and subsequent wound healing are initially affected by primary tissue damage, accompanied by lacerations or open wounds from the passage of age and suture thread [1-5].
To stabilize the wound, lembo are mobilized in order to facilitate their positioning, to promote primary healing. Suturing on the other hand reduces post-operative pain and increases patient comfort versus post-operative care. Suturing reduces the chances of infection in deeper tissues, such as the bone [1-5].
For the best possible clinical results, it is attempted against the perfect approximation of the wound lips, mainly as a primary element in periodontal aesthetic interventions and during regenerative procedures.
Sutures are usually placed initially distally to the last tooth, in each interproximal space, with continuous suturing in the mesial direction [1-5]. Suturing is initially applied to the more mobile approaches of periodontal tissue. The sign that the lips of the lembo are sufficiently aligned is the lack of tissue whiting, as the tissue approach is provided without restricting the blood supply to the lembo. Proper placement of surgical flaps contributes to patient comfort, and hemostasis, reducing wound size, and preventing unnecessary bone resorption. If the edges of the surgical wound are not properly aligned, hemostasis may be compromised and blood/serum may accumulate. This fact results in visible space between the soft tissue and the bone, which serves to delay the wound healing process [2,5-7].
The main factors in achieving the goal of optimal wound healing are suturing technique, type and diameter of suture material, type of surgical age and design of surgical node [3,4,7-13].
The classification according to the material of the most primary thread is that of dividing the thread into absorbable and non-absorbable, with the idea that if the suture needs to be removed from its place, or over time, it is absorbed by the tissue where it is placed. This element reduces the surgical dental treatment by another stage since the patient does not need to appear in the dental clinic for the removal of the suture threads and the absorption process needs a period of time that varies, but always starts over 7 days of placement in the oral cavity. Typically the absorption time ranges from 16 to 120 days, or even longer. The longer the absorption time of the suture thread, the longer the flap stays fixed to the edges of the surgical wound, continuously helping the healing process [2,5-7].
The study is oriented around the collection of already published data on the tensile strength of sutures most frequently used during the practice of periodontal surgery. The application of sutures always depends on the personal preferences and experience of the clinician who uses it and even this selection procedure is very routine without thinking about the individual characteristics of sutures that vary greatly depending on the type of suture material, beyond classification as absorbable and non-absorbable and whether or not a disinfectant solution should be used in the areas where the suture is applied.
The article is of the review type, presenting some data on the types of periodontal suturing, seen from the point of view of clinical advantages and disadvantages brought by the application of sutures selected on the basis of the needle, material, etc. The electronic search was performed in PubMed with the keywords: periodontal and suture, bacterial, and tensile strength. The combination of words is in the order mentioned above and the connecting word “and”. The time search interval is articles published in PubMed about periodontal sutures without a time limit.
Listed below are the types of sutures associated with the advantages and disadvantages in use.
imple interrupted suture
Inserted separately through the wound side.
Advantages:
- Strong and can be used in areas with pressure
- Placed 4 mm - 8 mm apart to close large wounds in such a way that the pressure is separated
- Each suture is independent and the removal of one suture will not vary with the removal of another suture.
- Easy to clean
Disadvantages:
- None
Simple continuous suture
A simple interrupted suture, the needle is inserted continuously so that the suture crosses perpendicular to the cutting line down and obliquely upwards. It ends by passing a knot over the unstressed edge of the suture.
Advantages:
- Fast technique which distributes the pressure in a uniform way.
Disadvantages:
- If it is cut at a point, the suture weakens along its entire length and makes possible the opening of surgical wounds.
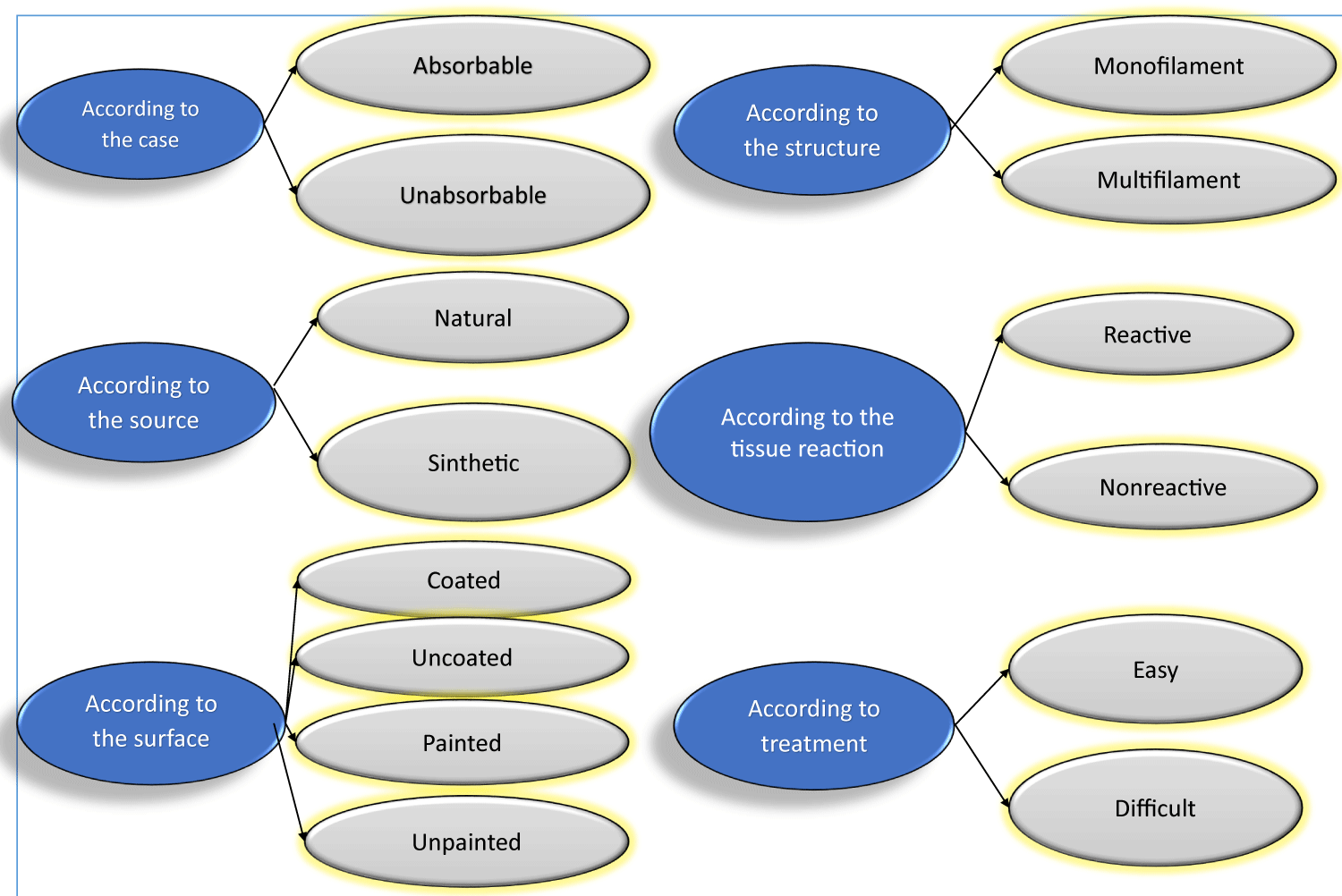
The data collected from the literature are presented in Table 1, which shows the classification of suture types based on the elements mentioned above.
Table 1: Data on suture types are classified on the basis of some distinguishing elements.
Surgical sutures are designed to place the suture into tissue with minimal tissue damage. There are 3 components: The end of the surgical needle, the body and the tip.
Surgical needle end: Suture is inserted into the needle through a hole through the end of the surgical needle. Surgical needles are atraumatic and act as a single unit [5,6,9-12].
Body Surgical Needle: The widest part of the surgical needle, which can be easily manipulated into large, superficial wounds and requires little wrist movement.
Surgical needle tip: Can be round/conical tip, triangular tip, etc.
The surgical needle holder should catch the surgical needle at approximately 1/3 of the distance from the end. A surgical needle should enter the tissue perpendicular to the surface. If the surgical needle pierces the tissue obliquely, the suture may rupture.
The suture should be placed at an equal distance from the incision on both sides and at equal depth. The surgical needle should pass from free tissue to fixed one. If one side of the tissue is thinner than the other, the surgical needle should pass from the thinnest tissue to the thickest one.
The distance that the needle passes through the tissue should be greater than the distance from the edge of the tissue [7,11,12].
Sutures should be placed approximately 3 mm - 4 mm apart.
ontinuous suture
Is similar to continuous suture, but closure is provided by pulling the suture through its loop. Indicated in areas of tuberosity and retromolar areas.
Advantages:
- Tightens multiple joints
- Distributes pressure evenly
- Waterproof closure
- Prevents excessive tightening
Disadvantages:
- Prevents the adjustment of pressure on the suture line after tissue swelling occurs.
Vertical suture
Covers in 2 levels, one deep to provide support and adhesion to the wound surfaces and one deep to pull the edges together. Used to close deep wounds [8,12,13].
Advantages:
- For better fit and maximum tissue approximation.
- Used to control soft tissue hemorrhage.
- Used for extra support where the wound will heal delayed for whatever reason.
Disadvantages:
- None
Horizontal suture
Avoids the borders of the mucosa, bringing larger areas of raw tissue in contact. It is mostly used for closing bone defects and cystic cavities [9,12,13].
Advantages:
- More used for closing bone defects or cystic cavities.
- Used to control bleeding after surgery from the gingiva around the tooth socket to stretch mucoperiosteal on the lower bone.
Disadvantages:
- Limits blood supply to the cutting edges.
- The needle is passed from one end to the other and again from the latter to form and bind a knot.
Cross suture (crisscross)
This suture is used on toothless spaces. Starting this technique, the needle penetrates the level of the mucogingival junction in the mesiobuccal line, goes horizontally under the flap, and emerges in the line of the distobuccal angle, the procedure is done at the lingual aspect, and suture material passes over the surgical field, connecting the suture node from the buccal aspect forming a cross on the flap [10,12,13].
Suture around a single tooth
The needle is first passed under the point of distal contact of the interdental papilla. The suture needle then penetrates the inside of the surgical flap raised 3 mm from the top of the papilla, the suture needle is passed back under the point of contact, then passed below the other point of contact in the mesial direction, and then the needle penetrates the surface of the suture, the inside of the surgically raised flap 3 mm from the tip of the interdental papilla, then the needle is passed back below the point of contact, tying the suture node but not in the raised tissue [10,12,13].
Periosteal suture
Periosteal suturing technique involves penetration into periodontal tissue/periosteum to bone. The needle is rotated backward in the direction it started as it penetrates the periosteum again, then passed through the keratinized tissue again [8]. A 180° rotation of the needle that catches the periosteum, the needle moves along the bone below the periosteum, and rotates around the body of the needle, allowing points to emerge from the periosteum and periodontal tissue [9,12,13].
Knowledge of sutures, needles (type, size, shape), suture instruments, and techniques are absolutely necessary to be a competent surgeon.
There is no better suturing than others in every aspect.
Differences in terms of tissue reaction and bacterial adhesion between sutures should always be taken into account in selecting the appropriate suture material.
Treatment during various delicate soft tissue suturing techniques can ensure optimal tissue healing and high aesthetic result.
Declarations
Availability of data and materials: The datasets analyzed during the current study are available from the corresponding author.
Acknowledgments belong to our family. Henri and Hera are our motivation for further in the field of scientific research.
Contributions
IR collected the scientific data and wrote the manuscript. SH revised and edited the manuscript. Literature research was conducted by SH and SK. GD and EK collected the scientific data. All authors read and approved the final manuscript.
Ethics declarations
Ethics approval and consent to participate: As the authors of the article, we state that there is no violation of the code of ethics during the realization of this article.
Consent for publication: Accepted.
- Silverstein LH. Essential principles of dental suturing for the implant surgeon. Dent Implantol Update. 2005 Jan;16(1):1-7. PMID: 15709717.
- Silverstein LH. Suture selection for optimal flap closure and tissue healing. Perio-implant showcase. Pract Periodontics Aesthet Dent. 2005; 16:2-3.
- Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Ann Surg. 1975 Feb;181(2):144-50. doi: 10.1097/00000658-197502000-00003. PMID: 122890; PMCID: PMC1343743.
- Zucchelli G, De Sanctis M. The coronally advanced flap for the treatment of multiple recession defects: a modified surgical approach for the upper anterior teeth. J Int Acad Periodontol. 2007 Jul;9(3):96-103. PMID: 17715841.
- Baldi C, Pini-Prato G, Pagliaro U, Nieri M, Saletta D, Muzzi L, Cortellini P. Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage? A 19-case series. J Periodontol. 1999 Sep;70(9):1077-84. doi: 10.1902/jop.1999.70.9.1077. PMID: 10505811.
- Newman M, Takei H, Klokkevold P, Carranza F. Newman and Carranza's Clinical Periodontology. 13th Edition - May 29, 2018; Contributor: Austin OSaben; eBook ISBN: 9780323533232; Hardcover ISBN: 9780323523004
- Kulkarni S, Dodwad V, Chava V. Healing of periodontal flaps when closed with silk sutures and N-butyl cyanoacrylate: a clinical and histological study. Indian J Dent Res. 2007 Apr-Jun;18(2):72-7. doi: 10.4103/0970-9290.32424. PMID: 17502712.
- Asher R, Chacartchi T, Tandlich M, Shapira L, Polak D. Microbial accumulation on different suture materials following oral surgery: a randomized controlled study. Clin Oral Investig. 2019 Feb;23(2):559-565. doi: 10.1007/s00784-018-2476-0. Epub 2018 May 2. PMID: 29717362.
- Varma SR, Jaber M, Fanas SA, Desai V, Al Razouk AM, Nasser S. Effect of Hyaluronic Acid in Modifying Tensile Strength of Nonabsorbable Suture Materials: An In Vitro Study. J Int Soc Prev Community Dent. 2020 Feb 5;10(1):16-20. doi: 10.4103/jispcd.JISPCD_343_19. PMID: 32181217; PMCID: PMC7055341.
- Abullais SS, Alqahtani NA, Alkhulban RM, Alamer SH, Khan AA, Pimple S. In-vitro evaluation of commonly used beverages on tensile strength of different suture materials used in dental surgeries. Medicine (Baltimore). 2020 Nov 25;99(48):e19831. doi: 10.1097/MD.0000000000019831. PMID: 33235053; PMCID: PMC7710252.
- Park JC, Koo KT, Lim HC. The hidden X suture: a technical note on a novel suture technique for alveolar ridge preservation. J Periodontal Implant Sci. 2016 Dec;46(6):415-425. doi: 10.5051/jpis.2016.46.6.415. Epub 2016 Dec 26. PMID: 28050319; PMCID: PMC5200867.
- Otten JE, Wiedmann-Al-Ahmad M, Jahnke H, Pelz K. Bacterial colonization on different suture materials--a potential risk for intraoral dentoalveolar surgery. J Biomed Mater Res B Appl Biomater. 2005 Jul;74(1):627-35. doi: 10.1002/jbm.b.30250. PMID: 15889436.
- Dragovic M, Pejovic M, Stepic J, Colic S, Dozic B, Dragovic S, Lazarevic M, Nikolic N, Milasin J, Milicic B. Comparison of four different suture materials in respect to oral wound healing, microbial colonization, tissue reaction and clinical features-randomized clinical study. Clin Oral Investig. 2020 Apr;24(4):1527-1541. doi: 10.1007/s00784-019-03034-4. Epub 2019 Jul 24. PMID: 31342245.