More Information
Submitted: July 13, 2022 | Approved: July 22, 2022 | Published: July 23, 2022
How to cite this article: Suguna Priya G, Shwetha P, Prafulla T. Evaluation of the health of temporomandibular joint – A novel technique. J Oral Health Craniofac Sci. 2022; 7: 005-009.
DOI: 10.29328/journal.johcs.1001037
Copyright License: © 2022 Suguna Priya G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Evaluation of the health of temporomandibular joint – A novel technique
Suguna Priya G1*, Shwetha Poovani2 and Prafulla Thumati2
1Post Graduate Student, Department of Prosthodontics, Rajarajeswari Dental College and Hospital, Bangalore, India
2Head of the Department, Department of Prosthodontics, Rajarajeswari Dental College and Hospital, Bangalore, India
*Address for Correspondence: Suguna Priya G, Post Graduate Student, Department of Prosthodontics, Rajarajeswari Dental College and Hospital, Bangalore, India, Email: [email protected]
Case report: This case report aimed to evaluate temporomandibular joint activity in a patient with the temporomandibular disorder before and after disclusion time reduction (DTR) therapy.
Results: Positive changes in joint health were observed in the patient after the DTR treatment.
Conclusion: The joint vibration analysis objectively showed significant results with the disclusion-time reduction therapy. The measured parameters were closer to the reference values. Thus, DTR is an effective method to treat TMJ disorders, based on Piper’s classification.
Temporomandibular joint disorders (TMD) are one of the complicated fields in dentistry [1]. It could manifest no other problem in different forms at any time during human life with symptoms such as limited mouth opening, pain in the TMJ area, pain in masticatory muscles, headache especially around the anterior temporal area, sounds emerging from temporomandibular joints, morning soreness, bruxism, clenching, head and neck pains, attrition and abfraction of teeth, internal derangement of temporomandibular disks, decrease in the volume of the synovial fluid [2].
In dentistry, no other problem must be managed multi-disciplinarily like TMJ disorders. Occlusal trauma that may occur after restorations is one of the biggest causes of temporomandibular joint disorders. Dental extraction and orthodontic restorations are also important conditions that cause this discomfort. Ideally, when there is no abnormality in a joint, no sound comes from that joint. There is no distortion in the relationship between the joint-disk-articular surface [3].
Normal joints produce very little friction and vibration. If there is degeneration in the joint, there is sound in the joint. The sound spectrum may be bigger or less than the human hearing limits. Scientific research has shown that TMJ sounds have been well categorized. Every TMJ sound is like a signature to a problem. Since sound is pressure energy, it has a particular frequency. Another kind of useful information source is a spectrum of TMJ sound. TMJ sounds have distinctive characteristics in clinical diagnosis efforts. Joint Vibration Analysis (JVA) is a computerized process of recording vibrations bilaterally from the TMJs and processing the vibrations in software to arrive at a reliable indication of whether the TMJs are normal or damaged. The recording step involves first measuring the range of motion (ROM) and denoting any deflection at a maximum opening of 3 mm or more. a pair of accelerometers are placed directly over the TMJs and the patient is instructed to open maximally and close to a light tooth contact 6 or more times. The patient follows an on-screen metronome to control the speed of the motion. This simple movement requires both condyles to translate to their full extent, revealing any limitation in the range of motion, deviations, deflection, and/or joint noises. The light tooth contact serves as a marker and verifies that the full ROM has been included within the recording. The patient must follow the instructions such as the opening to maximum, closing all the way to light tooth contact, and following the pacing of the metronome to produce a useable joint vibration (JVA) record [4].
Occlusal equilibration had been advocated by numerous authors as a successful treatment modality. However, some authors contend that myofascial pain dysfunction syndrome (MPDS) is a stress-related disorder that was not brought about by occlusal factors. The lactic acid then accumulates over time as these prolonged excursive contacts continually hyperactivate the involved musculature, thereby producing the ischemic symptomatology often seen in the MPDS subject.
DTR is to quickly disclude the posterior teeth in less than 0.5 seconds per excursion, primarily in right and left excursions and secondarily in protrusive excursions.
Hence the present study was undertaken to evaluate the temporomandibular joint vibrations before and after (DTR) therapy in a patient with temporomandibular disorders using (JVA).
A 34-year-old female patient was referred to the department of Orofacial Pain with the chief complaint of pain during mouth opening, on the left side of TMJ for 4 months with no relevant medical history. On clinical examination, it was manifested that the mouth opening was 31 mm with a deviation towards the left side of 3 mm and the palpatory findings revealed tenderness of the left lateral pterygoid, masseter, and medial pterygoid, clicking sounds heard on auscultation.
Based on the above complaint and clinical examination provisional diagnosis was Acute disc dislocation, non-reducing (Piper’s 4b). To confirm the diagnosis, JVA was carried out as a chairside investigation, it was directly connected to the circuit using a computer that works on BIOJVA software.
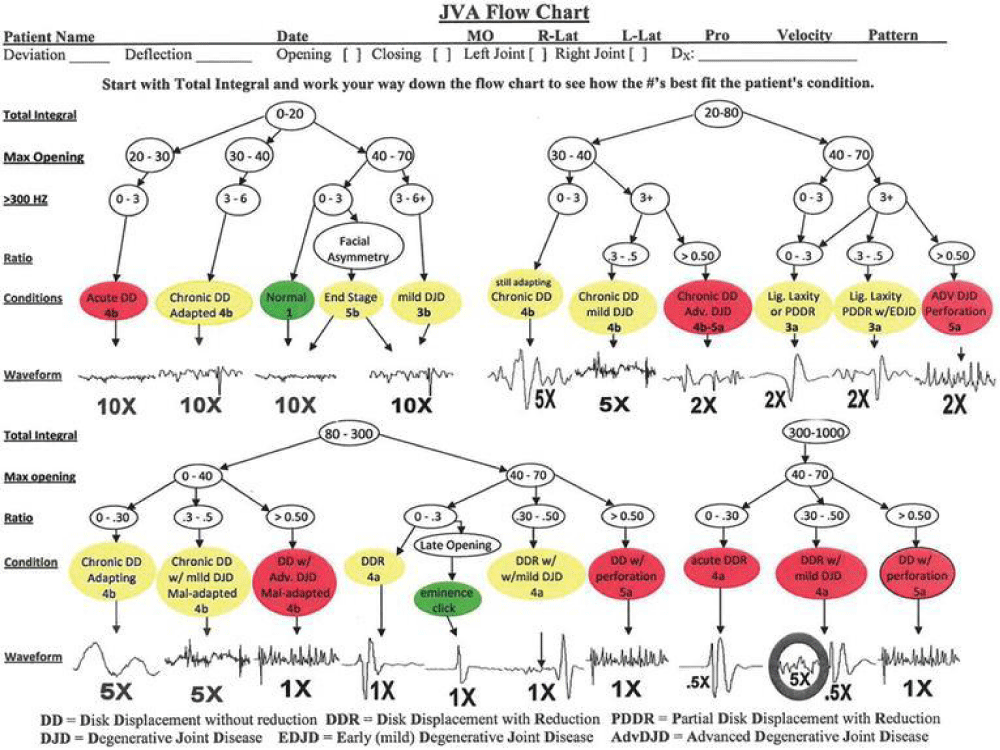
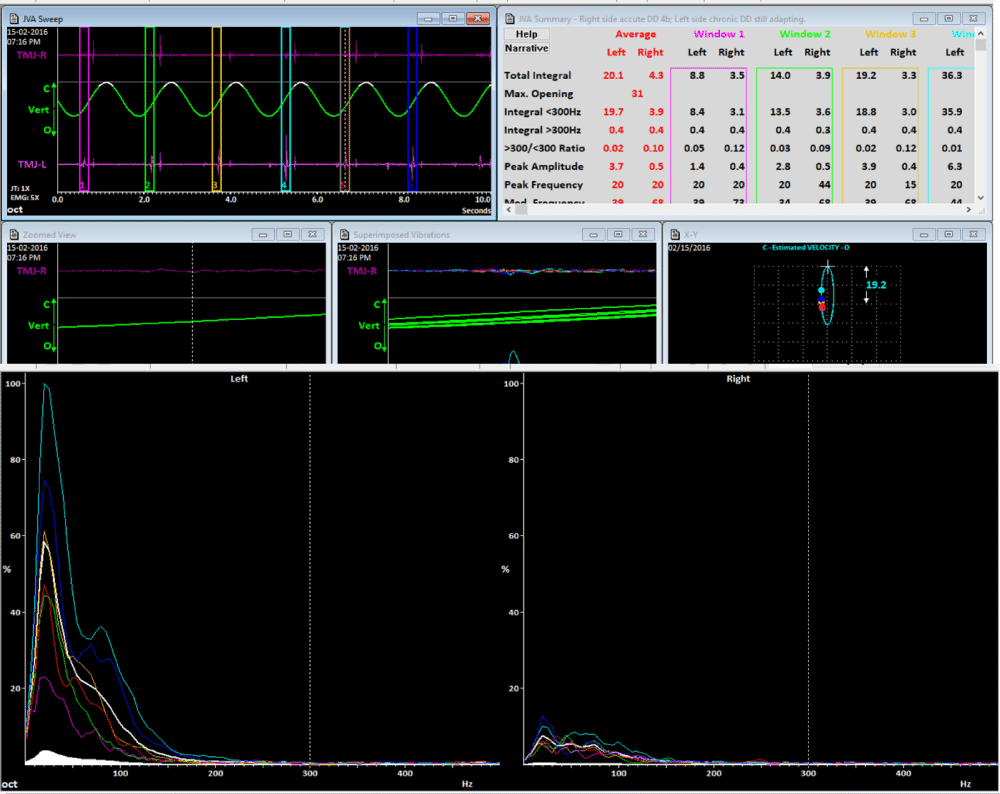
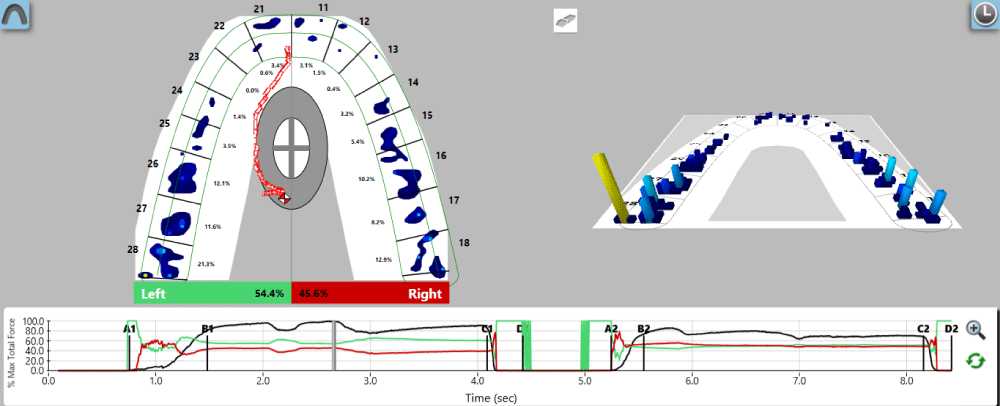
The software (Biopak, BioResearch, Inc., Milwaukee, WI, USA) paired with the device allows for the specification of each reported vibration. The requirement for a reliable and correct single registration is a repeatable translation of both condyles to their full extent-provided by a repeatable pre-declared range of the mouth opening-and the subsequent subtle intermaxillary occlusal contact during the clenching of both dental arches, coupled with the action of the metronome. Full condylar movements reveal limitations in the range of mandibular motion, deviations, deflections, and potential temporomandibular vibrations. The subtle intermaxillary occlusal contacts facilitate verification of the maximum mandibular range of motion included in the single registration. It was placed over the patient’s head at the level of the TMJ area and a metronome was displayed on the system which guides the patient in opening and closing cycles. The movements were analyzed using BIO PAK software and evaluated using Mark Piper’s classification where specific waveforms of vibrations were analyzed. By correlating the JVA standard values in the flow chart (Figure 1) with the patient JVA values (Figures 2,3) the provisional diagnosis was Chronic Disc Displacement with Reduction. Treatment: An orthotic was fabricated and after 3 weeks of active treatment and follow-up showed an increased mouth opening of 55 mm and a reduced deviation of 1 mm. Post -JVA values showed no vibrations on opening and closing (Figures 4,5).
Figure 1: JVA flowchart
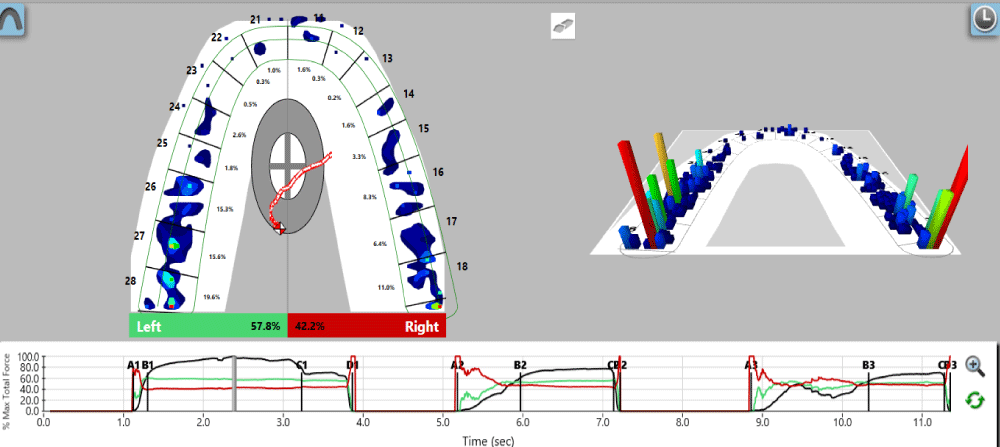
Figure 2: Multibite analysis before DTR therapy, showing long diclusion time.
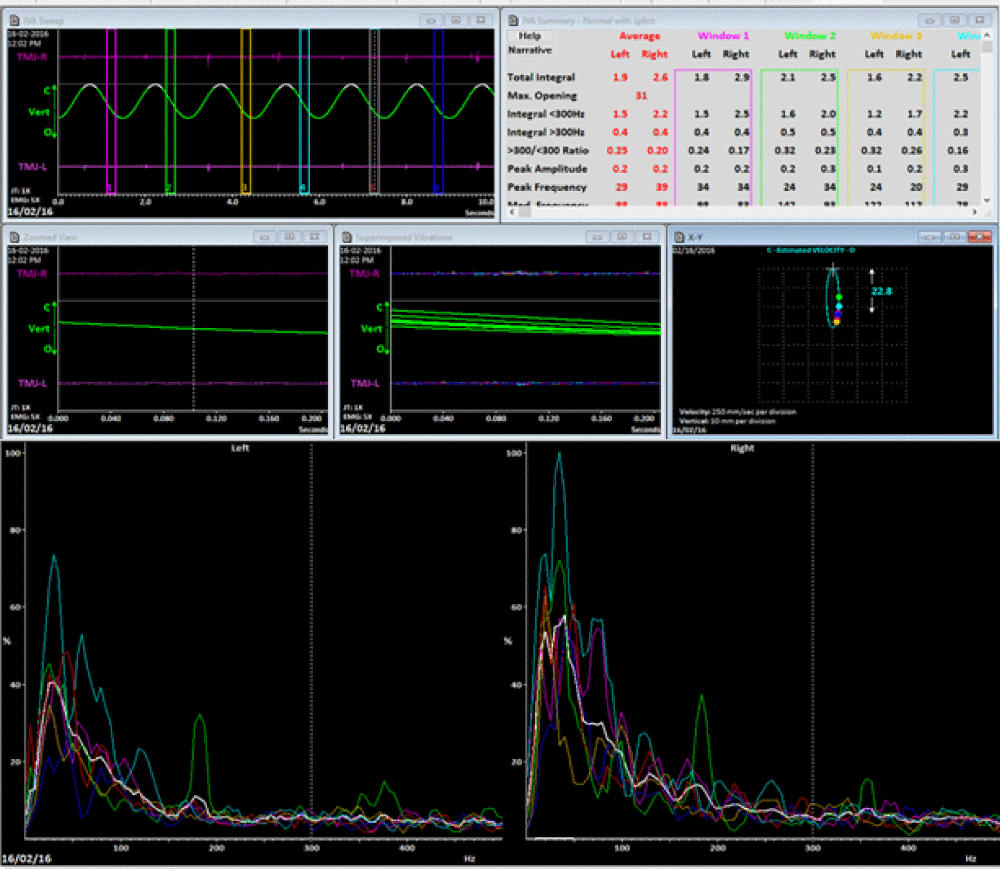
Figure 3: Pre-treatment wavelet and FFT waveform JVA record showing medium intensity vibrations on the left side typical of a chronic disk displacement with reduction. The right TMJ seems to be within the normal limits as the Total Integral is less than 20.
Figure 4: Multibite analysis after DTR therapy showing shortened diclusion time.
Figure 5: Post-treatment wavelet and FFT waveform JVA record from the same subject as in although vibrations are still present, they are reduced to within normal limits and the left TMJ in this subject has remained so
Temporomandibular joints, masticatory muscles, teeth, bones, and the central nervous system are all involved in TMJ pathology. For many years, clinicians have employed various mechanical tools for diagnosis and to understand the reasons for the problem. There are several diagnostic aids to evaluate TMJ health. Due to the development of the chipset technology and software programming, we have now device-based diagnostic tools, joint vibration analysis, joint tracking measuring mastication analysis, computer-based occlusal analysis devices, and so on available. These device-based technologies require studying with a new methodology. Joint vibration analysis and finally digital occlusal analysis systems all need new methodologies.
A study conducted by Ahmed, et al. in 2009, stated that as a part of the Multisite Research Diagnostic Criteria For Temporomandibular Disorders (RDC/TMD) Validation Project, comprehensive temporomandibular joint diagnostic criteria were developed for image analysis using panoramic radiography, magnetic resonance imaging (MRI), and computerized tomography (CT). In this study, the reliability of the radiologists was poor in interpreting panoramic radiographs for TMD [5].
A systematic review of the literature on the efficacy of MRI in diagnosing TMJ disorders showed that the results from the literature are inconsistent and that the evidence is insufficient. A systematic review indicated that cone beam CT (CBCT) may be superior to multidetector CT, although the reviewers suggested that further studies were needed to determine the usefulness of CBCT compared with multidetector CT.
In a recent systematic review, the diagnostic validity of such instrumentation used to measure and characterize this phenomenon must be tested using research designs with strong foundations including reliable evidence, blinded examiners, an acceptable reference standard such as MRI, and acceptable psychometric properties. They concluded that the excellent reliability obtained by the examiners reading the JVA data demonstrated that examiners could be trained and reliably identify and interpret the pertinent data produced by this technological device.
According to a study published by Prafulla Thumati, et al. in 2014, a computer-analyzed occlusal equilibration procedure called immediate complete anterior guidance development (ICAGD) to reduce disclusion time by either reduction or addition has been described in the literature. It has been shown to reduce muscle hyperactivity and successfully treat the symptoms of TMD. The ICAGD procedure was only possible to perform because of the time measurement capability of the T-Scan occlusal analysis system. ICAGD is a computer-guided, measured coronoplasty based on specific tome-based numerical occlusal endpoints [6].
Studies conducted by various authors have suggested that DTR is an effective treatment modality in reversing mild TMD conditions such as Mark Piper’s classification. It can be inferred that JVA is an effective tool to diagnose the health of the TMJ and DTR therapy is an effective treatment for TMD. The results showed a significant difference in the joint vibrations after DTR therapy [7-12].
Therefore, every TMJ is unique, no two JVA records will ever be the same. While certain parameters have general characteristics, there will always be a few exceptions. Therefore, it can be concluded that TMJ vibration analysis using BioJVA allows for the detection of early or latent dysfunction of the temporomandibular joint.
The advent of disclusion time reduction therapy using properly performed DTR therapy is a potentially new direction in the treatment of TMD (Mark Piper’s classification) and was quite successful in the treatment.
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008 Dec 18;359(25):2693-705. doi: 10.1056/NEJMra0802472. PMID: 19092154.
- Issa TS, Huijbregts PA. Physical therapy diagnosis and management of a patient with chronic daily headache: a case report. Journal of Manual & Manipulative Therapy. 2006; 14(4):88E-123E
- Prinz JF, Ng KW. Characterization of sounds emanating from the human temporomandibular joints. Arch Oral Biol. 1996 Jul;41(7):631-9. doi: 10.1016/s0003-9969(96)00070-2. PMID: 9015563.
- Kerstein RB. Disocclusion time-reduction therapy with immediate complete anterior guidance development to treat chronic myofascial pain-dysfunction syndrome. Quintessence Int. 1992 Nov;23(11):735-47. PMID: 1305288.
- Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Jun;107(6):844-60. doi: 10.1016/j.tripleo.2009.02.023. PMID: 19464658; PMCID: PMC3139469.
- Thumati P, Manwani R, Mahantshetty M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. Cranio. 2014 Oct;32(4):289-99. doi: 10.1179/2151090314Y.0000000004. Epub 2014 Apr 30. PMID: 25252768.
- Thumati P, Kerstein RB, Thumati RP. Disclusion time reduction therapy in treating occluso-muscular pains. J Indian Prosthodont Soc. 2017 Jan-Mar;17(1):95-98. doi: 10.4103/0972-4052.194948. PMID: 28216853; PMCID: PMC5308075.
- Sharma S, Crow HC, Kartha K, McCall WD Jr, Gonzalez YM. Reliability and diagnostic validity of a joint vibration analysis device. BMC Oral Health. 2017 Feb 16;17(1):56. doi: 10.1186/s12903-017-0346-9. PMID: 28209141; PMCID: PMC5314607.
- Brown DT, Cox LK 2nd, Hafez AA, Cox CF. "True normal" TMD control subjects: a rare clinical finding. Cranio. 1998 Apr;16(2):84-9. PMID: 9709562.
- Radke J, Yiannios N, Sutter B, Kerstein R. TMJ vibration changes following immediate complete anterior guidance development. Advanced Dental Technologies & Techniques. 2018; 31:5018.
- Giray B, Sadry S. Modifications in Class I and Class II Div. 1 malocclusion during orthodontic treatment and their association with TMD problems. Cranio. 2019 Feb 11.
- Ramachandran A, Jose R, Tunkiwala A, Varma R B, M Shanmugham A, Nair PK, Kumar KS, Sam LM. Effect of deprogramming splint and occlusal equilibration on condylar position of TMD patients - A CBCT assessment. Cranio. 2021 Jul;39(4):294-302. doi: 10.1080/08869634.2019.1650216. Epub 2019 Aug 26. PMID: 31451061.