Case Report
Clinical Case: Necrotizing Fasciitis of the neck after surgery of a Mandibular Radicular Cyst

Egils Kornevs* and Normunds Bauers
Riga Stradins University, Student Faculty of Dentistry, Department Oral and Maxillofacial Surgery, Riga, Latvia*Address for Correspondence: Egils Korņevs, Riga Stradins University, Department Oral and Maxillofacial Surgery, Associate Professor, REUH (Riga East University Hospital) Latvian Oncological Center Surgical Clinics Oral and Maxillofacial Surgeon, Riga, Latvia, Tel: 371 4555523; Email: [email protected]
Dates: Submitted: 13 November 2017; Approved: 23 November 2017; Published: 24 November 2017
How to cite this article: Kornevs E, Bauers N. Clinical Case: Necrotizing Fasciitis of the neck after surgery of a Mandibular Radicular Cyst. J Oral Health Craniofac Sci. 2017; 2:110-117. DOI: 10.29328/journal.johcs.1001020
Copyright License: © 2017 Kornevs E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Odontogenic infection; Necrotizing fasciitis
Abstract
Introduction
Necrotizing fasciitis (NF)-infection of soft tissues that results in destruction of fascia and soft tissues. The infection spreads over subcutaneous tissues and fascia, but relatively preserving muscle tissue. Infections that occur in the region of head and neck, in most cases the etiology is odontogenic. Two types of necrotizing fasciitis are the most common. The first type is caused by mixed anaerobic bacteria and facultative microorganisms (Streptococci and Enterobacteria). The second type is group A Streptococci. The disease typically has fast progression, systemic toxicity that can even cause death of the patient. Occasionally it is called the “flesh-eating bacteria syndrome”. The early stages of the infection are characterized as pain that is not accompanied by changes in the skin. Erythema, swelling, cellulitis and occasionally crepitation shows up gradually (relatively quickly, in 1-2 days). The local infection is accompanied by systemic symptoms. The pain is accompanied by a fever, tachycardia, and diaphoresis, sometimes a change in the mental condition or diabetic ketoacidosis. The diagnosis is determined by a careful examination of the patient, and finding out the site of entry and the cause of infection- skin inflammation of a certain body part. Improper diagnosis and the following treatment can cause death from sepsis, mediastinitis and hemorrhage of carotid artery, v. Jugularis interna thrombophlebitis or aspiration pneumonia. For the treatment the use of wide spectrum antibiotics, aggressive surgical tactics and supportive therapy is accepted. Histologically characteristic feature is necrosis of superficial fascia, thrombosis of blood vessels. The presence of inflammatory cells differentiates this pathology from clostridial myonecrosis. Obliterating vascular thrombosis, polymorphonuclear infiltration is seen in the profound layers of the superficial fascia. Necrosis sets in the subcutaneous fat, air in the interfacial space, vascular thrombosis with following changes in the skin.
Case Report
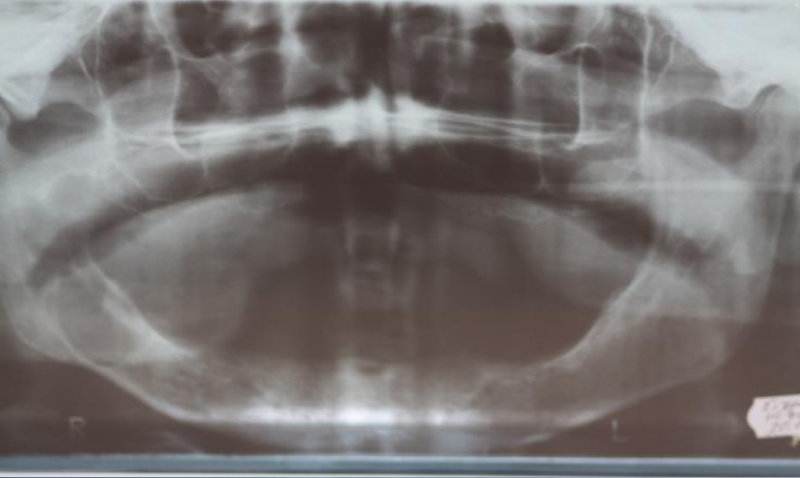
A.E 72-year-old man, was treated in the department of head and neck surgery of RECUH (Riga East Clinical University Hospital) LOC (Latvian Oncological Center) with diagnosis: Cysta mandibula dxt. Complication: Phlegmona colli bilateralis (Necrotizing fasciitis). The patient came to the clinic with complaints about a lesion in the right side of the mandibula, and secretions from the lesion. According to anamnesis morbi, the patient believes that everything started in January 2009, when he felt an increasing mass and secretions in his mouth, and that his mandibular complete denture didn’t fit him as well as before. In July 2010, the patient went to the Institute of Stomatology department of surgery, where radiographically he was diagnosed with a cystic lesion that was punctured. Cytological examination diagnosed a cyst with a secondary inflammation. Patient was informed about the need for surgery, but he declined for family reasons. In 22.10 2010 the patient had an exacerbation of the inflammation, that manifested as facial asymmetry and an increase of secretions in the mouth, beforehand the patient had visited a private dental practice where he received an incision that released a purulent discharge. The patient was given a mouth wash, and post operation antibacterial therapy- Amoxiclav 625mg 3 times a day, as well as analgesic therapy- Ibuprophen 400mg 3 times a day. In a week, there was a noticeable decrease in the volume of the formation, but the patient still was bothered with the constant discharge from the wound, that’s why he went to the department of maxillofacial surgery at the Center of Oncology of Latvia. There was a noticeable asymmetry of the face due to the swelling of the left cheek. A noticeable formation was seen intraorally on the edentulous arch, it was located in the molar, retromolar and ascending ramus region. When palpating the wound, a cloudy discharge was noticed. Radiographically in the panoramic image a well-defined cystic lesion was noticed in the right side of the mandibular corpus and lower third of the ascending ramus (Figure 1).
The patient was assigned for a surgical treatment at the department of head and neck surgery at the Center of Oncology of Latvia, where he was stationed at 23.11.2010, at the hospital there were no changes in local state of the patient. The patient recalls from his medical history, that he had heart rhythm disturbances that were treated with Cordarone pills, he noted that he sometimes had an increased blood pressure that he controlled with Betaloc pills. The patient is a chronic smoker- he smokes 10-15 cigarettes a day. The overall condition of the patient was good. Blood pressure 130/80 mmHg, pulse 65x min. The blood tests showed a decreased amount of neutrophil leucocytes 31.1%, an increase of lymphocytes 59.4%. The hemostasis indicators were without a deviation. An increased level of cholesterol 5.51 mmol/l. The patient was prepared for surgery in general anesthesia at 24.11.2010. On the morning of 24.11.2010 at 7AM the patient received premedication of Dormicum 7.5mg, Ranitidin 150mg and 30 minutes before surgery Promedol 2% 1ml, and Atropine 0.1%-0.5ml. The patient underwent a cystectomia mandibula dextra. At the beginning of surgery, the patient received 1g of Cefazoline i/v and Dexazone 12mg. A crestal incision was made on the right side of the lower third of ramus ascendens, retromolar and molar region. A mucoperiosteal flap and an opening in the resorbed bone was made to ensure a good field of vision of the surgical site. When access to the cyst was enlarged- 5ml of serous-purulent discharge was released from the wound. After the extirpation of the cystic lining, the bone cavity was rinsed with 0.2% chlorhexidine, a hemostatic sponge was inserted to control the bleeding. The wound was closed with 4-0 vicryl sutures without a drainage. The cystic lining was sent to histological examination. Postoperatively the patient received Cefazoline i/v injections- 1000mg 3 times a day, Diclofencaum natricum 75mg-3ml x2, and 0.2% chlorhexidine mouthwash. Histological results- after surgery NR152053/10- Cyst was lined with squamous epithelium that was infiltrated with chronic inflammation cells. Possibly a radicular cyst.
On the day after surgery the patient complained about mild pain that resided after receiving analgesics, overall status of the patient was good. Locally an increased volume of the right cheek region, the tissues palpated were soft and swollen. There was no discharge from the wound, hygiene of the mouth was satisfactory. Third day after the surgery (Saturday- the treating physician didn’t check up on the patient, but the patient was taken care by the on-call doctor and nurses) in the morning the patient felt pain and noticed an increase of the right cheek, the right submandibular region was affected as well. An extra therapy of Tramadol 100mg i/m two times a day was assigned. On Sunday, the on-call doctor consulted the patient. The overall condition of patient was satisfactory- T- 37C, TA- 140/70mmHg. No respiratory disturbance was noticed. Locally an increase of the submental and right submandibular region, with hyperemia of the skin. Extra analgesics were prescribed. On the fifth day after surgery the treating physician examined the patient and noticed an increase of volume of the right cheek, right submandibular, submental, and right and left region of the neck, that went over to the anterior thoracic wall. The skin was warm with red/purple regions, in some places erosions, ulcers and pustules were found. On palpation crepitation was felt. Patient complained about persisting pain that wasn’t responding to the analgesic therapy, fever, weakness and loss of appetite (Figure 2).
Temperature 37.5C. Blood tests showed erythrocyte sedimentation rate of 40mm/h, Leukocytes 17.7 103/mm3, Erythrocytes-3,55L 10mm3. Hemoglobin 11,3g/dl, hematocrit 32.2%, Neutrophil 60, Meta 1, Micro+, Lymphocytes 4, Aniso+. CRP 162mg/l, bicarbonate 134.6mmol/l. taking the clinical and blood tests in account, a new diagnosis was set- cellulitis. Extra USG was made for the neck. In the USG- on the right anterior side of the neck from submandibular to clavicular region- multiple small dense formations were seen, that were more or less mobile. The USG results fit the diagnosis of cellulitis of the neck. During general anesthesia 3 horizontal incisions were made on the right side and 2 horizontal incisions were made on the left side of the neck. A purulent, necrotic discharge was released from the wound, the material was sent for microbiological examination, the wound was irrigated with chlorhexidine solution and five drainages were placed. The patient was moved to the intensive care unit. An aggressive antibacterial therapy was initiated: Dalacin C 1200mg x2, Metrogyl- first dose 15mg/kg, further 500mg every 8 hours. Isotonic sodium chloride 1000ml, gelofuzine 500ml and glucose 500ml i/v infusion was made. Dexamethazone 12mg was injected for its anti-inflammatory, anti-allergic and analgesic properties. Diazepamum 0.5% -5ml injections in the evenings before sleep. Next day after surgery overall status of the patient was satisfactory: T37.1 C, TA-120/80mmHg, patient didn’t complain about difficulties to breathe or swallow, pain was mild and was gone after analgesics. There was no noticeable change of the enlarged area, the skin around the incisions had necrotic regions, and the wounds had a purulent, necrotic discharge. The wounds were irrigated and drainages were placed (Figure 3).
The wounds were taken care of daily, necrectomies were made, and the irrigation was done while patient was sedated, due to the pain. The cleansing of the wounds took about 2 weeks, the patient was in a moderately serious condition. Clinically intoxication with subfebrile temperature was noted, changes in the blood tests: ESR 40mm/h, WBC12, 7H103/mm3, RBC-3.55L 10mm3. HGB-10,6L g/dl, hematocrit-32.2L%, Neutrophyls-60, Meta 1, Micro+, Lymphocytes-4, Aniso+. Microbiological tests results from the incision wounds- E. coli 100 million colonies per ml, Enterococcus sp. 500000 colonies per ml. Hafnia alvei 5 million per ml. Staphylococcus coagulase negative 1000 colonies per ml. Candida. Enterococcus sensitive to Ampicillin, Hernia sensitive to Ciproflexane, E. Colli sensitive to Ampicillin. All were sensitive to Gentamycin. Fluconazole, Apimicillin, Gentamicin and Ceftriaxon was prescribed. On the 14th day after the surgery the overall condition of the patient was severe. Patient had pain, temperature up to 38.6C. Swelling appeared locally on the right upper third of the anterior thoracic wall, while palpating the tissues crepitation was felt. During an i/v narcosis, incision was made in the swollen region, purulent discharge was released, the wound was irrigated and drainage was placed (Figure 4).
After the incision, the overall status of the patient got better, but after four days the patient complained about diarrhea. Fecal microbiological tests were made. Test results- Clostridium Difficile A/B toxin- negative. The diarrhea was related to the use of antibiotics. The use of Cefazoline and Gentamycin was discontinued. Irrigation of the wound continued for three weeks after the surgery. On the 20th day after the surgery the wound was clean and was actively granulating. The overall status of the patient was getting better, temperature was normalizing. The blood tests were improving as well- Erythrocytes- 3,92L 10mm3, Hemoglobin -11.8 L g/dl, Leukocytes 6.6 103 mm3, lymphocytes 20.7, ESR 13 mm/h. On the 25th day after the surgery the wounds were clean and actively granulating. The overall status of the patient was good (Figure 5).
It was taken into account that there was a large skin defect, to speed up the healing process, a skin transplantation was offered to the patient. The patient didn’t agree to the proposal. After 10 days, the patient returned to the hospital with necrotic margins of the wounds. The small lesion (2cm in diameter) was excised under local anesthesia. The discharge from the wound was sent for microbiological examination. The results showed Psudomonas aeruginosa- 100000 colonies per ml, Staphylococcus coagulase negative- 100000 colonies per ml. After being hospitalized the patient had complaints about abdominal pain. The consulting surgeon suspected possible gastritis due to prolonged time antibiotics and analgesics were used. Fibro-gastroscopic examination was assigned. FGS results was duodenal ulcer, insufficiency of cardia, hyperemic gastropathy. On the 10th day the patient was released from the hospital. The wound continued to granulate, and after 3 months the wound was completely closed (Figure 6).
Discussion
Even though necrotizing fasciitis is a rare condition (up to 2,6% of all infections in the head and neck region), dentists, ENT-doctors, maxillofacial surgeons, need to be informed about the symptoms of the disease, its progression, risk factors, causative factors, diagnostic criteria, treatment tactics and the possible complications. Infections that manifest in the region of the head and neck, in most cases are of odontogenic origin [1-4]. The main cause of this disease is a non-vital tooth or pericoronitis (from partially erupted 3rd molar), complications after tooth extractions, periapical granulomas and infected cysts. Post-surgery trauma, defects related to fractures, salivary gland disorders, lymph node diseases, infection that is related to the use of local anesthesia. It is diagnosed more often in the extremities, abdominal wall, and perineum, and less frequently in the region of head and neck. Joseph Jones in 1871 was first to use the term “Hospital gangrene”. In 1918 Pfanner called a similar condition, caused by hemolytic streptococci “Erysipelas necroticans [5]. The first time the term “Necrotizing fasciitis” was used was in 1952 by Wilson to describe a widespread necrosis of a superficial fascia (Wilson B) [6]. This term has been well established. In most cases this disease is of multimicrobial nature. The microorganisms using their toxins and enzymes travel from subcutaneous tissues over the superficial and profound fascia. The infection causes blood vessel occlusion, ischemia and thrombosis. M1 and M3 surface proteins improve the microorganism adhesion to the hosts cells, and protect from phagocytosis. The streptococcal pyrogenic exotoxins release cytokines and cause hypotension. The disease progresses faster in patients with diabetes, chronic kidney insufficiency, immunocompromising diseases, patients with surgical traumas and patients undergoing radiation therapy. The diagnosis is based on clinical signs that initially can be hard to notice, that’s why the diagnosis is set in the late stages of the disease, which results in comparatively high mortality [7-11]. In this case one of the major factors that had a role in the spreading of the infection was the infected cyst that was treated with antibiotics. The prolonged periods of antibiotic use might have a role in the evolution of resistant microorganisms. Based on the cause the disease can be divided in 5 types. The 1st type-Polymicrobial origin- Group a Streptococcus and anaerobic bacteria and/or facultative anaerobic bacteria. This kind of microbial flora is often seen after trauma or surgery. Subdermal fat and superficial facia are affected but muscle tissues are preserved, gasses are formed. 2nd type is caused by group A streptococcus: only Streptococcus pyogenes or in combination with Staphylococcus aureus. The background of this infection is cause by the toxic shock caused by Streptococci. 3rd type Clostridial myonecrosis: scrotal fasciitis that is characterized by formation of gasses. 4th type Fournier (1883) [12] gangrene: necrotizing oropharyngeal infection with secondary V.jugularis interna thrombophlebitis and metastatic infection. Caused by Fuscobacterium necrophprium. In most cases the pathogenic bacteria enter through skin wounds or surgical wounds. 5th type Lemmierre syndrome [13]: gangrene is characterized by rapid development. The main signs are muscle necrosis and gas formation. The most frequent causative bacteria is Clostridium perfringens. Possible predisposing factors are trauma, surgery or Varicella infection. In the presented case, the microbiological results from the discharge of the incision wound showed E. coli 100 million colonies per ml, Enterococcus sp. 500000 colonies per ml. Hafnia alvei 5 million per ml. Staphylococcus coagulase negative 1000 colonies per ml. Enterobacteria were the most common. These bacteria can be found in the oral cavity and on the skin. In most cases the infection develops 2-4 days after the initial damage. Six clinical symptoms characterize the development of the disease. 1. Necrosis of the superficial fascia and detachment of the surrounding tissues. 2. Systemic toxic reactions with changes of the mental state. 3. Muscles aren’t affected. 4. Clostridium species aren’t isolated. 5. No occlusion in the peripheral arteries is seen. 6. Pathological examinations of the necrotic tissues show a massive infiltration of leukocytes, focal necrosis of superficial fascia and surrounding tissues, and thrombosis of microcirculatory blood vessels. In our case local swelling and pain was noticed on the third postsurgical day. Initially the patient’s health status didn’t show any signs that a dangerous and aggressive infection would start. T 37, TA 140/70mmHg. No changes in the respiratory system were noticed. The patients’ mental status wasn’t affected. Due to the fact that the patient visited the hospital on the weekend, and his health was assessed by an on-call doctor. Since the doctor wasn’t a maxillofacial surgeon, the diagnosis wasn’t set adequately. On the fifth postsurgical day, the patient’s condition was severe. The maxillofacial surgeon noticed a diffuse swelling in the right cheek, right submandibular and submental regions, that extended into the anterior thoracic wall. Crepitation was felt when the tissues were palpated. Patient complained about fatigue, fever, weakness and severe pain, that wasn’t responsive to the prescribed analgesics. From all the laboratory tests, 6 serologic results are the most important [14] LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) -C reactive protein, white blood cells, hemoglobin, bicarbonate, creatinine and glucose. These criteria are evaluated by a scale: CRP mg/L >150: 4 points. Leukocytes (x103/mm3) <15:0 points, 15-25:1 point, >25:2 points. Hemoglobin (g/dl) >13.5:0 points, 11-13.5:1 point, <11:2 points. Glucose (mmol/L) >10:1 point. If the indicator has 6 or more points, the risk of necrotizing fasciitis is very high. The laboratory results of our patient were indicating necrotizing fasciitis. Leukocytes 17.7 103/mm3, CRP-162mg/L, Hemoglobin-11,3g/dl. Bicarbonate 134.6 mmol/L. Even though the glucose and creatinine levels were normal, the LRINEC test results were 8 points. From all the radiological examinations, the CT was considered the most significant and informative. The status of the pathologic process and upper airways can be evaluated with CT [15]. We didn’t use this examination due to technical difficulties, but the situation demanded immediate surgical intervention. Even though ultrasonography isn’t considered a good diagnostic tool for necrotizing fasciitis, we used this examination method to confirm the diagnosis. The treatment consists of aggressive surgery with evacuation of necrotic tissues, antibacterial therapy. The discharge from the wound and blood have to get tested to provide an effective antibacterial therapy. The bacteriological tests showed that Enterococcus was sensitive to Ampicillin, Hafnia alvei to Ciproflexane, E. Colli to Ampicillin. All were sensitive to Gentamycin. These antibiotics were used, and proved to be effective. The side effect of the antibacterial therapy was enterocolitis. Appropriate changes in the antibiotics made it possible to avoid further complications. The wound has to be inspected daily, the necrotic tissues have to be excised until the wound starts to actively granulate. Adequate intensive care is important to maintain normal metabolic processes of the patient- feeding, fluid and electrolyte substitution. Unfortunately, in some cases septic shock can occur, that can cause destruction of multiple organs and lead to a lethal outcome. After the start of or quicker healing and scar tissue prophylaxis, reconstructive skin transplantation is advised. In our case the patient declined our offer for a skin transplantation. Nevertheless, after the wound tissue scarred, the patient didn’t mention any functional or cosmetic defects.
Conclusions
Necrotizing fasciitis is one of the most dangerous infectious complications in the region of head and neck. Aggressive surgery, effective antibiotic treatment targeting the cause of the infection, regular care of the wound, greatly reduces the risk of a life-threatening complication.
Summary
The clinical report of the necrotizing fasciitis encourage to keep in mind:” Where is surgery, there are complications”. Due to the radicular cyst, the patient underwent a cystectomy, which in maxillofacial surgery is considered a routine procedure. On the third day after the surgery (which was a weekday, and the patient was inspected by on call doctors) first symptoms were noticed- pain and swelling of the left cheek and submandibular region. The overall was critically assessed by the fifth day, where local and general symptoms of necrotizing fasciitis were severe. The diagnosis was confirmed with clinical examinations, laboratory tests, and ultrasonography. Extensive bilateral incisions of the neck, broad spectrum antibiotics and active intensive care of the patient saved the patient’s life.
References
- Tung-Yiu W, Jehn-Shyun H, Ching-Hung C, Hung-An C. Cervical necrotizing fasciitis of odontogenic origin: a report of 11 cases. J Oral Maxillofac Surg. 2000; 58: 1347-1352. Ref.: https://goo.gl/Cozer2
- Lin C, Yeh FL, Lin JT, Ma H, Hwang CH, et al. Necrotizing fasciitis of the head and neck: an analysis of 47 cases. Plast Reconstr Surg. 2001; 107: 1684-1693. Ref.: https://goo.gl/RCxmFH
- Schütz P, Joshi RM, Ibrahim HHH. Odontogenic necrotizing fasciitis of the neck and upper chest wall. J Oral Maxillofac Surg Med Pathol. 2012; 24: 32-35. Ref.: https://goo.gl/nHM883
- Lorenzini G, Picciotti M, Di Vece L, Emanuela P, Leopoldo B, et al. Cervical necrotizing fasciitis of odontogenic origin involving the temporal region-a case report. J Craniomaxillofac Surg. 2011; 39: 570-573. Ref.: https://goo.gl/RgKjjj
- Weiss A, Nelson P, Movahed R, Clarkson E, Harry Dym. Necrotizing fasciitis: review of the literature and case report. J Oral Maxillofac Surg. 2011; 69: 2786-2794. Ref.: https://goo.gl/vQjLJo
- Wilson B. Necrotizing fasciitis. Am Surg. 1952; 18: 416-431. Ref.: https://goo.gl/R14myA
- Hefny AF, Eid HO, Al-Hussona M, Idris KM, Abu-Zidan FM. Necrotizing fasciitis: a challenging diagnosis. Eur J Emerg Med. 2007; 14: 50-52. Ref.: https://goo.gl/nmQBxB
- Lee JW, Immerman SB, Morris LG. Techniques for early diagnosis and management of cervicofacial necrotising fasciitis. J Laryngol Otol. 2010; 124: 759-764. Ref.: https://goo.gl/dvfuyX
- Díaz Manzano JA, Cegarra Navarro MF, Medina Banegas A, López Meseguer E. Diagnostico y tratamiento de la fascitis necrotizantecervical. Evolucion tras una angina de Ludwig. An OtorrinolaringolIbero Am. 2006; 33: 317-322. Ref.: https://goo.gl/1tAwSd
- Lindner HH. The anatomy of the fasciae of the face and neck with particular reference to the spread and treatment of intraoral infections (Ludwig's) that have progressed into adjacent fascial spaces. Ann Surg. 1986; 204: 705-714. Ref.: https://goo.gl/zbu9w7
- Bono G, Argo A, Zerbo S, Triolo V, Procaccianti P. Cervical necrotizing fasciitis and descending necrotizing mediastinitis in a patient affected by neglected peritonsillar abscess: a case of medical negligence. J Forensic Leg Med. 2008; 15: 391-394. Ref.: https://goo.gl/jvZ4dN
- Thwaini A1, Khan A, Malik A, Cherian J, Barua J. Fournier's gangrene and its emergency management. Postgrad Med J. 2006; 82: 516-519. Ref.: https://goo.gl/LK5f3J
- Lemierre. On certain septicemias due to anaerobic organisms. Lancet. 1936; 1: 701-703. Ref.: https://goo.gl/53zhnQ
- Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC ( Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care med. 2004; 32: 1535-1541. Ref.: https://goo.gl/TjU8qm
- Becker M, Zbären P, Hermans R, Becker CD, Marchal F, et al. Necrotizing fasciitis of the head and neck: role of CT in diagnosis and management. Radiology. 1997; 202: 471-476. Ref.: https://goo.gl/se7jTx